In 2025, dental implants are becoming increasingly accepted worldwide, and the technology is continuously advancing. According to research from the International Team for Implantology (ITI), the 5-year success rate of dental implants exceeds 95%. However, some patients still face the risk of implant failure.
So, why do dental implants fail? The primary causes of failure include poor osseointegration, infections, and excessive stress, all of which can often be mitigated with proper preventive measures.
This article will analyze dental implant success rate statistics, explore common clinical causes of failure, and provide 10 key factors on how to prevent dental implant failure to help both doctors and patients improve the long-term stability and success of dental implants.
Key Factor 1: Patient Selection and Preoperative Evaluation
Successful dental implant procedures begin with accurate patient selection and thorough preoperative evaluation. The criteria for dental implants typically include sufficient bone volume, good oral health, and the absence of severe systemic diseases.
Bone density is a crucial factor in determining implant stability. A study published in the Journal of Oral Implantology shows that patients with low bone density have a significantly higher implant failure rate compared to those with adequate bone volume. Therefore, conducting a bone density assessment before surgery is essential. CBCT scans can precisely assess the quality of the jawbone, ensuring that the implant receives sufficient bone support.
Additionally, medical contraindications for dental implants also play a vital role in success rates. For instance, implant failure rates are nearly twice as high in patients with uncontrolled diabetes compared to the general population. Smokers face an even higher risk, with failure rates increasing by more than three times due to the negative effects of nicotine on osseointegration and delayed healing. Therefore, before surgery, it is essential for doctors to thoroughly evaluate the patient’s medical history and take targeted measures, such as controlling blood sugar levels and encouraging smoking cessation, to improve the long-term success rate of dental implants.
Key Factor 2: Implant Design and Material Selection
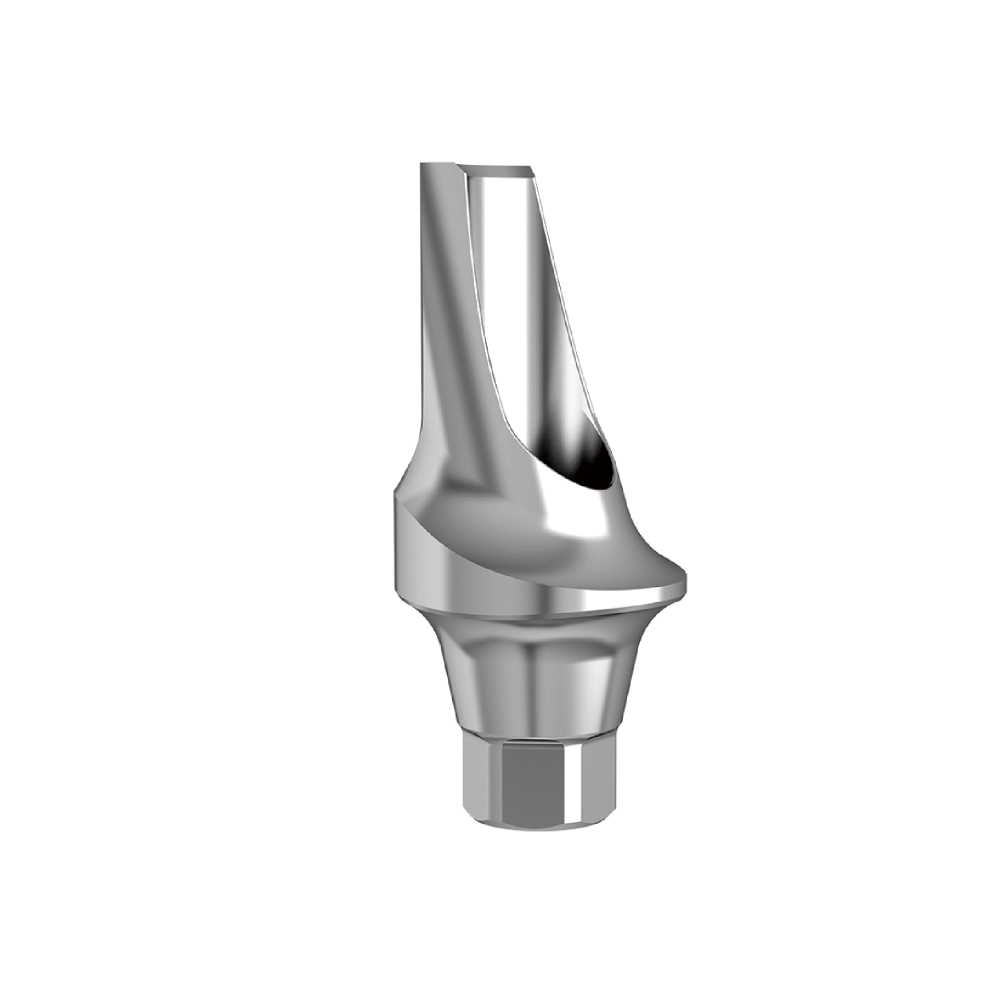
In the field of dental implants, the design and material selection of the implant play a decisive role in the success of the surgery and the long-term experience for patients. Currently, titanium alloy and zirconia are two commonly used materials for implants. Titanium alloy offers excellent mechanical properties and good biocompatibility. Its high strength allows it to withstand substantial biting forces, and it is less prone to deformation or fracture in the complex mechanical environment of the oral cavity. This makes titanium alloy a widely used material for implants. However, the metallic color of titanium alloy implants may have aesthetic limitations, especially for patients who require high aesthetic standards, such as those needing implants in the anterior region.
Zirconia implants, on the other hand, have a significant advantage in aesthetics, as they closely resemble natural teeth in color and exhibit outstanding aesthetic performance. They also offer good biocompatibility and corrosion resistance. However, zirconia implants are more challenging to process, come at a higher cost, and, in terms of mechanical strength, are slightly inferior to titanium alloy. When exposed to excessive biting forces, zirconia implants have a higher risk of chipping.
In addition to the material itself, the surface treatment technology of implants is crucial for osseointegration. For example, SLA (Sandblasted Large-grit Acid-etched) technology creates a rough, porous surface on the implant, increasing the contact area between the implant and bone tissue. This facilitates the adhesion, proliferation, and differentiation of bone cells, accelerating the osseointegration process and improving implant stability. Hydrophilic coating treatments alter the wettability of the implant surface, enabling blood and tissue fluid to spread quickly across the surface, promoting early cell adhesion and growth. This significantly shortens the healing time of the implant, especially in patients with poor bone quality or those who require faster healing.
In 2025, numerous well-known brands, such as Nobel and Straumann, have made significant advancements in implant design and material research. With their mature technologies and reliable quality, these brands hold an important position in the market. They continually optimize their products by incorporating advanced materials and surface treatment technologies into implant design, offering patients better and more reliable dental implant solutions.
Key Factor 3: Precision in Surgical Planning
Successful dental implant placement relies heavily on meticulous preoperative planning to ensure accuracy, safety, and long-term stability. Advances in digital dentistry for implant placement have revolutionized treatment protocols, making procedures more predictable and reducing complications. Among these advancements, CBCT scans for dental implants and computer-guided surgery play a crucial role in improving precision.
The Role of CBCT in Implant Surgery
Cone Beam Computed Tomography (CBCT) has become an indispensable tool in implant planning, offering three-dimensional imaging that provides detailed anatomical insights. Unlike traditional two-dimensional X-rays, CBCT scans for dental implants allow clinicians to assess bone volume, bone density, nerve positioning, and sinus location with high accuracy. Studies have shown that preoperative CBCT analysis significantly reduces implant failures by ensuring proper angulation, depth, and positioning of the implant fixture. This imaging technology is especially critical in complex cases, such as posterior maxillary implants where proximity to the maxillary sinus poses risks, or mandibular implants where the inferior alveolar nerve must be carefully avoided.
Guided Surgery: Enhancing Accuracy and Safety
The use of guided implant surgery accuracy has transformed traditional freehand implant placement into a highly precise, minimally invasive technique. Surgical guides, created based on digital treatment planning, help in transferring the virtual implant plan to the patient’s mouth with near-perfect accuracy. A study published in the Journal of Oral and Maxillofacial Surgery found that guided implant surgery reduces deviation in implant positioning by over 50% compared to freehand methods, leading to better primary stability, optimal prosthetic outcomes, and lower complication rates.
Avoiding Nerve and Vascular Damage
One of the greatest risks in implant surgery is nerve and blood vessel injury, which can result in numbness, pain, or excessive bleeding. Proper CBCT assessment and digital surgical guides help in precisely mapping out implant sites to avoid critical anatomical structures such as the inferior alveolar nerve, mental foramen, and sinus cavities. Additionally, utilizing depth control systems and dynamic navigation technology further enhances precision, ensuring safe and accurate placement while minimizing surgical trauma.
With the continuous advancements in digital dentistry for implant placement, clinicians can now achieve higher success rates, shorter recovery times, and improved patient satisfaction. Integrating CBCT technology, guided surgery, and digital workflow into implantology is no longer an option but a necessity for predictable, long-lasting implant success.
Key Factor 4: Aseptic Techniques and Infection Control
In dental implant surgery, strict aseptic techniques and effective infection control are crucial for ensuring surgical success and maintaining patients’ oral health. Peri-implantitis prevention is a top priority, and the appropriate use of antibiotics plays a significant role in this process.
Preoperative and Postoperative Use of Antibiotics
Before surgery, the decision to use antibiotics depends on the patient’s specific condition, such as the presence of systemic diseases or the risk of local oral infections. Following the guidelines for antibiotic prophylaxis for dental implants, the necessity, type, and dosage of antibiotics should be carefully determined. For patients with a standard risk profile, preoperative prophylactic antibiotics may not be required. However, for high-risk patients, such as those with diabetes or cardiovascular diseases, the appropriate use of antibiotics before surgery can help reduce the risk of postoperative infections. Similarly, postoperative antibiotic use should be adjusted based on the patient’s recovery status, and prolonged use should be avoided to prevent antibiotic resistance.
Sterilization Standards in the Operating Room
The disinfection and sterilization of the surgical environment are also of paramount importance. According to the American Dental Association (ADA) sterilization protocols in implantology, all surgical instruments must undergo thorough cleaning, disinfection, and sterilization. Before the procedure, the operating room should be meticulously cleaned and disinfected using methods such as ultraviolet (UV) irradiation and chemical disinfectant wipes to ensure a sterile surgical environment. During surgery, medical professionals must strictly adhere to aseptic protocols, including wearing sterile surgical gowns, gloves, and masks. After the procedure, the operating room and all used instruments must be re-sterilized to prevent cross-contamination.
By rigorously implementing these aseptic techniques and infection control measures, the risk of infection in dental implant surgery can be significantly reduced, thereby increasing the success rate of implants and providing patients with a safe and reliable treatment experience.
Key Factor 5: Bone Augmentation Techniques
In dental implant procedures, when a patient has insufficient bone volume, bone augmentation techniques become a key method for ensuring the success of the implant. Sinus lift for dental implants is an effective solution for insufficient bone volume in the posterior maxillary region. The alveolar bone in this area is located just below the maxillary sinus, and with aging or prolonged tooth loss, the bone volume in this region often becomes severely inadequate for direct implant placement. Sinus lift surgery involves elevating the mucosa of the maxillary sinus and placing bone grafting material between the sinus floor and the alveolar ridge, increasing the bone height and providing sufficient bone support for the implant.
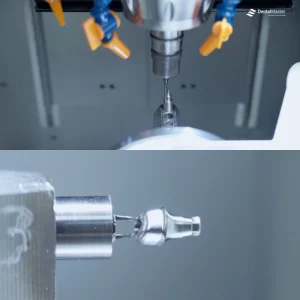
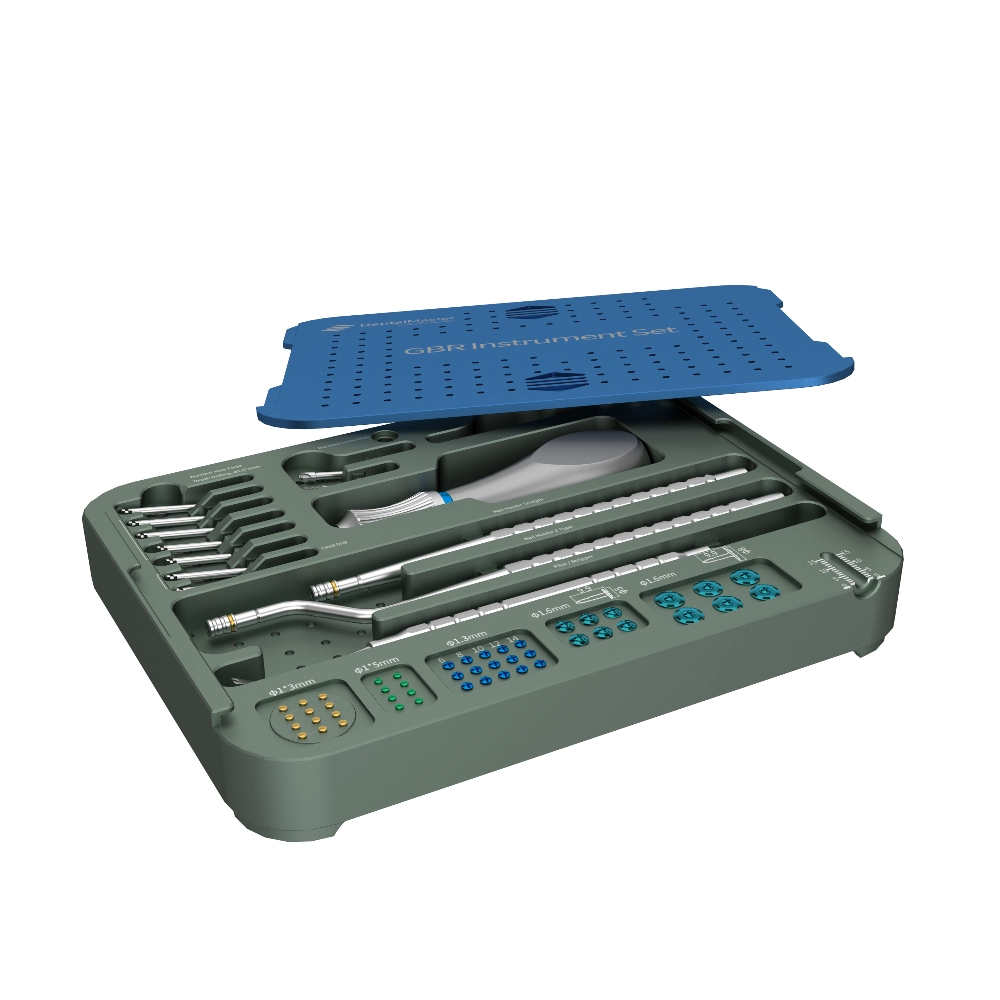
Guided Bone Regeneration (GBR) is suitable for various bone defect situations. It utilizes the barrier function of a biological membrane to prevent soft tissue cells from entering the bone defect area, guiding osteogenic cells to migrate preferentially to the defect site and promoting new bone formation. Our company offers specialized sinus lift kits and GBR kits, which include a range of precision instruments needed for surgery to assist the clinician in performing the procedure accurately.
When selecting bone grafting materials, autografts, and synthetic bone each have their own characteristics. Autografts, taken from the patient’s own body, such as from the iliac crest or mandible, offer unmatched biocompatibility and osteoinductive properties, providing the best bone formation results. However, the downside is that they require a second surgical site, increasing patient discomfort and surgical risk, with limited donor bone availability. Synthetic bone materials, such as hydroxyapatite and tricalcium phosphate, are widely available and can be processed into different shapes and sizes according to needs. They avoid the trauma associated with bone harvesting and offer a stable physicochemical structure that serves as a good scaffold for new bone growth. However, synthetic bone has relatively weaker osteoinductive properties compared to autografts.
In clinical practice, clinicians will select the most appropriate bone graft material and bone augmentation technique based on the patient’s specific condition, such as the extent of bone defects and overall health, to achieve the best possible dental implant outcome.
Key Factor 6: Initial Stability of the Implant
The initial stability of the implant is a crucial foundation for the success of dental implants, directly affecting the implant’s ability to achieve osseointegration in the alveolar bone and maintain long-term function. The Implant Stability Quotient (ISQ) and implant insertion torque are key indicators used to assess the initial stability of the implant. The ISQ measures the stability of the implant using resonance frequency analysis, with higher values indicating better stability. Implant insertion torque reflects the resistance encountered during implant placement, and the appropriate torque ensures a close fit between the implant and bone tissue.
Surgical techniques play a key role in enhancing the initial stability of the implant. For instance, controlling the drilling diameter is essential to ensure good contact between the implant and bone tissue. If the drilling diameter is too large, the gap between the implant and the bone wall will increase, leading to insufficient mechanical retention, which negatively impacts initial stability. On the other hand, if the drilling diameter is too small, excessive compression on the bone tissue during implant placement can cause bone necrosis, which also compromises initial stability. Our DentalMaster DMD dental implants are designed with compatibility with various surgical techniques in mind, helping clinicians precisely control the surgical procedure and improve implant stability. Notably, DentalMaster DMD dental implants are fully compatible with Nobel implants, offering more options and convenience for clinicians, and are also suitable for immediate loading, significantly reducing the time patients are without teeth and improving their quality of life.
When it comes to the timing of loading the implant, both immediate loading and delayed loading have their own indications. Immediate loading refers to the placement of a temporary restoration and the application of a certain amount of occlusal force immediately after implant insertion. The advantage of immediate loading is that it allows the patient to quickly regain chewing function and aesthetics; however, it requires very high initial implant stability. This method is typically used when the bone quality is good, the implant insertion torque reaches a certain standard, and there is no significant inflammation around the implant. Delayed loading, on the other hand, involves a healing period after implant insertion, during which the implant forms a strong bond with the bone before it is subjected to loading. This approach is more conservative and is suitable for cases where the bone quality is poor, initial implant stability is insufficient, or the patient’s overall health is compromised. Clinicians will assess the patient’s specific situation, such as bone density, implant initial stability, and overall health, and choose the most suitable loading method to ensure the long-term success of the dental implant.
Key Factor 7: Soft Tissue Management & Aesthetics
In the field of dental implants, soft tissue management and aesthetics are crucial aspects that directly affect both the patient’s treatment experience and long-term outcomes. The gingival biotype plays a significant role in the long-term aesthetic results of implant dentistry. Gingival biotypes are generally classified into thin and thick biotypes. The thin biotype has thinner gums, less connective tissue, and clearly visible blood vessels. While it may appear more delicate aesthetically, it carries a higher risk of gingival recession after implant surgery. Once gingival recession occurs, exposing the neck of the implant not only affects the aesthetics but may also lead to peri-implantitis, disrupting the balance of soft and hard tissues around the implant. On the other hand, the thick biotype has thicker gums with abundant connective tissue, offering better protection around the implant and significantly reducing the likelihood of gingival recession, maintaining a stable aesthetic result in the long term.
Soft tissue grafting techniques have a wide range of applications in implant procedures. Connective tissue grafting is a commonly used method of soft tissue transplantation. When a patient experiences gingival recession, insufficient soft tissue around the implant, or requires improvement in the aesthetic appearance of the implant area, connective tissue grafting plays a critical role. For instance, after implant placement, if the surrounding gingiva is found to be too thin, the dentist can take an appropriate amount of connective tissue from other areas in the patient’s mouth (such as the palate) and graft it around the implant. This increases the gingival thickness, enhances the quality and shape of the soft tissue, reduces the risk of gingival recession, and improves the pink aesthetics around the implant, ensuring that the surrounding gingiva blends more harmoniously in color and shape with natural teeth. Additionally, for patients already experiencing peri-implant mucositis, combining soft tissue grafting techniques while controlling inflammation helps repair damaged tissues and restore a healthy environment around the implant, ensuring its long-term stability and aesthetic outcome. Through appropriate soft tissue management and aesthetic considerations, it is possible to create implant restorations that are both functional and aesthetically pleasing for patients.
Key Factor 8: Occlusal Load Management
Occlusal load management is one of the key factors for the success of dental implants, directly affecting the implant’s lifespan and the patient’s oral health. Following the correct implant occlusion principles is crucial for dispersing occlusal forces and preventing occlusal overload.
Take a middle-aged patient as an example. Shortly after dental implant restoration, the patient experienced implant loosening. A detailed examination revealed that improper adjustment of the occlusal relationship after the restoration caused the implant to bear excessive occlusal forces, resulting in occlusal overload. Prolonged overload led to excessive pressure on the bone tissue surrounding the implant, which gradually caused bone resorption and ultimately resulted in implant loosening. The solution to this issue was first to readjust the occlusal relationship, reshaping the restoration to ensure that the occlusal forces were evenly distributed between the implant and surrounding natural teeth. Additionally, the patient was advised to avoid eating hard foods in the short term to reduce the load on the implant and give the surrounding bone tissue time to recover. After a period of observation and care, the implant’s stability gradually returned.
For patients with bruxism, this is a potential risk factor for implant failure. During nocturnal teeth grinding, the teeth are subjected to abnormal, excessive occlusal forces. These forces repeatedly impact the implant, which can easily cause damage to the surrounding bone tissue, accelerating implant loosening and potentially leading to implant loss. For such patients, the recommended solution is to wear a night guard for implant protection. The night guard effectively cushions the forces generated during teeth grinding, reducing the abnormal load on the implant. In addition, dentists need to guide patients on oral hygiene, as bruxism may cause bacteria to proliferate in the mouth, leading to inflammation and affecting the health of tissues around the implant. Regular follow-ups are also essential to detect and address any potential issues in a timely manner, ensuring the implant can function stably over the long term. Through scientific and reasonable occlusal load management, the success rate and longevity of dental implants can be significantly improved, providing patients with higher-quality oral restoration outcomes.
Key Factor 9: Postoperative Maintenance and Follow-up
Postoperative maintenance and follow-up are critical for ensuring the long-term success of dental implants. They directly affect the implant’s lifespan and the patient’s oral health. Proper postoperative care can effectively extend the service life of the implant and improve the patient’s quality of life.
For home care, mastering the correct dental implant cleaning techniques is crucial. It is recommended to use a water flosser for assistance in cleaning. The water flosser, utilizing high-pressure pulsating water streams, can deeply clean the gaps around the implant and surrounding gums, removing food debris and plaque, thereby reducing the risk of peri-implantitis. Brands like Waterpik and Bissell offer water flossers with adjustable settings to meet different patients’ cleaning needs. Additionally, a soft-bristled toothbrush is essential for daily cleaning, as its soft bristles can prevent damage to the implant surface and surrounding gum tissues. The Bass brushing technique should be used to ensure that every tooth surface is effectively cleaned. After brushing, using dental floss further helps to remove debris between the teeth.
Regarding follow-up visits and imaging examinations, long-term implant maintenance requires regular check-ups. Generally, after implant surgery, routine follow-ups should be scheduled at 1 week, 1 month, 3 months, and 6 months. Afterward, based on the stability of the implant and the patient’s oral health, follow-up visits can be scheduled every six months or annually. During each visit, in addition to routine oral examinations, the doctor may arrange for imaging tests such as X-rays or CBCT scans. Through these imaging tests, the doctor can clearly observe the integration between the implant and the surrounding bone tissue, and promptly detect issues such as bone resorption or implant loosening, so that appropriate treatment measures can be taken. Regular postoperative maintenance and follow-up allow both the doctor and the patient to work together to protect the health of the implant and ensure its long-term functionality.
Key Factor 10: Surgeon Expertise and Teamwork
In the field of dental implants, surgeon expertise and teamwork are among the core elements determining the success or failure of dental implant surgeries. How to choose an implant dentist is a crucial step for patients to achieve successful dental implant restoration. A large amount of research data shows that surgeon experience has a significant impact on the success rate of dental implants. A study published in an authoritative oral medicine journal indicates that surgeons who have completed more than 500 dental implant surgeries can achieve a success rate of over 95%; while for surgeons with insufficient experience, who have completed less than 100 dental implant surgeries, the success rate is only around 80%. Abundant clinical experience enables surgeons to more precisely deal with various complex oral anatomical structures and unexpected situations that may occur during surgeries. For example, when handling complex cases such as insufficient bone mass and proximity to the maxillary sinus, experienced surgeons can rely on their exquisite techniques and keen judgment to formulate more reasonable surgical plans, thereby effectively improving the success rate of dental implants.
The importance of multidisciplinary implant teams is also of great significance. Take an actual case as an example. A patient suffered from anterior tooth loss due to trauma, accompanied by severe alveolar bone defect. During the treatment process, the surgeon first performed an alveolar bone augmentation surgery to create conditions for the subsequent implant placement. Subsequently, based on the patient’s oral condition, facial aesthetics, and functional requirements, the prosthodontist closely communicated with the surgeon to jointly determine the implantation position, angle, and depth of the implant. After the implant was successfully implanted and healed, the prosthodontist carefully fabricated a dental crown that highly matched the color and shape of the patient’s natural teeth, restoring the patient’s aesthetics and masticatory function. Throughout the entire process, the surgeon, prosthodontist, and other relevant department staff worked closely together, giving full play to their respective professional advantages. In order to maintain and enhance the professional level of the team, doctors also actively participate in various dental implant training courses, continuously learning cutting – edge implant technologies and concepts, so as to provide patients with higher – quality and more reliable dental implant treatment services. It can be seen that excellent surgeon expertise and efficient teamwork are powerful guarantees for the success of dental implants.
Conclusion
In the field of dental implants, numerous factors work together to determine the success or failure of treatment. The ten key factors we have discussed, from meticulous patient selection and comprehensive preoperative assessments to strict postoperative care and maintenance, each play a vital role. Accurate patient selection, thorough evaluation of bone density, and careful consideration of medical contraindications lay a solid foundation for the implant procedure. Choosing the appropriate implant material, surface coatings that promote osseointegration, and advanced bone augmentation techniques such as sinus lift and guided bone regeneration (GBR) meet the physiological requirements for successful implantation.
A sterile operating procedure, effective infection prevention, and strict control of the surgical environment ensure the health of the implantation site. Establishing initial implant stability, managing occlusal loads properly, and handling soft tissues appropriately contribute to the long-term functionality and aesthetics of the implant. In addition, the professional skills of the dentist, seamless teamwork of the dental team, and continuous professional development through training courses are crucial for achieving the best treatment outcomes.
Personalized treatment is particularly important. Each patient has unique oral conditions, overall health status, and lifestyle factors. Tailoring the implant treatment plan according to these individual characteristics can significantly improve success rates and patient satisfaction.
Looking ahead, emerging technologies are expected to further enhance the success rate of dental implants. Artificial intelligence can be used to analyze vast amounts of patient data, predict potential complications, and optimize treatment plans. 3D printing technology can create customized implants and surgical guides, ensuring more precise fits and better integration with the patient’s anatomical structure. These technological advances, along with the continuous improvement of clinical techniques and a deeper understanding of the biology related to implants, will undoubtedly lead to more successful dental implant treatments in the future. In conclusion, by following the key success factors and embracing future technological trends, the dental implant field will provide better oral health solutions for patients worldwide.
Frequently Asked Questions about Dental Implants
Q: Can a failed dental implant be replaced?
A: It is possible to replace a failed dental implant. There are many reasons why dental implants may fail, such as poor osseointegration, peri-implantitis, and occlusal trauma. Once a failure is determined, the doctor will conduct a thorough evaluation of the cause. If the failure is due to insufficient bone volume, a bone augmentation procedure, such as guided bone regeneration (GBR) or sinus lift surgery, may be needed before the new implant can be placed to provide sufficient bone support. If peri-implantitis is the cause, the inflammatory tissue must be thoroughly removed and the infection controlled. After the inflammation subsides and the oral environment stabilizes, re-implantation can be considered. However, the success rate of re-implantation is influenced by various factors, including the patient’s health, local oral conditions, and the reasons for the initial implant failure.
Q: How long does a dental implant last?
A: The lifespan of a dental implant varies from person to person. Generally, with proper maintenance, dental implants can last for over 10 years, or even a lifetime. The longevity of the implant depends on several factors:
- The patient’s oral conditions and overall health, such as good oral hygiene, stable periodontal health, and the absence of serious systemic diseases (e.g., uncontrolled diabetes), which help prolong the lifespan of the implant.
- The material and quality of the implant. High-quality implants typically have better biocompatibility and mechanical properties, allowing them to function longer in the mouth.
- Postoperative maintenance and care. Regular check-ups, proper cleaning (such as using a water flosser or soft-bristled toothbrush), and avoiding excessive force when chewing hard foods can significantly extend the implant’s lifespan.
Q: What is the success rate of dental implants in smokers?
A: The success rate of dental implants in smokers is relatively lower. Research indicates that the failure rate of implants in smokers is more than three times higher than in non-smokers. This is primarily due to harmful substances like nicotine in tobacco, which affect the osseointegration process between the implant and bone tissue. Nicotine reduces local blood circulation, decreases osteoblast activity, and inhibits bone matrix synthesis, which delays bone healing and increases the risk of implant loosening and failure. Additionally, smoking can worsen oral hygiene, leading to peri-implantitis and further threatening the stability of the implant. Therefore, smokers who are planning to undergo dental implant surgery are advised to quit smoking before the procedure to improve the success rate.
Q: Does dental implant surgery hurt?
A: Dental implant surgery is generally painless. Prior to the procedure, the doctor will administer local anesthesia to numb the surgical area. However, once the anesthetic wears off, there may be mild pain and discomfort, similar to the feeling after a tooth extraction. This pain is usually tolerable, and most patients can effectively relieve it by taking standard pain medications. Postoperative pain and swelling can vary from person to person, but they typically subside over a few days. If the pain is severe or persists for a long time, it is important to contact the doctor for further evaluation.
Q: What should I pay attention to after getting a dental implant?
A: After receiving a dental implant, it is essential to maintain good oral hygiene. Avoid brushing your teeth within the first 24 hours post-surgery. After that, use a soft-bristled toothbrush and follow the correct brushing method (such as the Bass method) to clean your teeth, along with using a water flosser to remove food debris and plaque around the implant. In terms of diet, avoid eating hard or sticky foods in the short term to prevent excessive force on the implant or loosening of the crown. It is also crucial to follow your doctor’s instructions regarding regular follow-up visits. Generally, routine check-ups should be scheduled 1 week, 1 month, 3 months, and 6 months after surgery, and thereafter based on the stability of the implant, every six months or annually. During these visits, the doctor will check the stability of the implant, the health of the surrounding gums, and may perform imaging tests to detect and address any potential issues early.