This clinical case presents a challenging scenario involving horizontal block bone augmentation in the maxilla with simultaneous implant placement in a partially edentulous patient. The complexity lies not only in the need to reconstruct deficient alveolar bone horizontally but also in addressing the esthetic demands of the anterior region and the limited residual bone height beneath the maxillary sinus at site #16. Key surgical considerations included achieving adequate flap tension release to prevent soft tissue compression and graft resorption, maintaining long-term peri-implant health in a thick gingival biotype, and optimizing implant angulation to maximize bone-to-implant contact in areas of limited sinus height. This case highlights a comprehensive, multidisciplinary approach to achieving functional and esthetic success in complex maxillary implant rehabilitation.
PREOPERATIVE CBCT IMAGING ANALYSIS
Site #12: Mean alveolar ridge width – 3.43 mm
Site #14: Mean alveolar ridge width – 4.27 mm
Site #13: Mean alveolar ridge width – 3.82 mm
Site #16: Mean alveolar ridge width – 6.81 mm
Average residual bone height to the floor of the maxillary sinus – approximately 6.85 mm


Diagnosis and Treatment Plan
Diagnosis
- Partial edentulism in the region of teeth #12 to #16
- Insufficient horizontal alveolar bone volume across the #12–#16 region
Treatment Plan
A horizontal block bone augmentation procedure will be performed across the #12 to #16 area to restore adequate ridge width. Simultaneously, four dental implants will be placed at the corresponding sites to restore function and aesthetics. This combined surgical approach aims to enhance bone volume, ensure primary stability of the implants, and reduce overall treatment time.
Surgical Procedure
Stage I Surgery
Four DentalMaster DMD implants were placed in conjunction with horizontal block bone augmentation in the maxillary #12–#16 region, followed by submerged healing.
- Local Anesthesia and Flap Elevation:
After achieving sufficient local anesthesia, a crestal incision was made and a full-thickness mucoperiosteal flap was reflected to expose the alveolar ridge.

- Horizontal Block Bone Augmentation with Simultaneous Implant Placement:
In the edentulous maxillary region spanning teeth #12 to #16, a horizontal ridge augmentation was performed using block grafts to increase ridge width. Simultaneously, four DentalMaster DMD implants were strategically placed to ensure optimal positioning and primary stability. The grafts were then stabilized and the surgical site was closed for submerged healing.

Stage II Surgery
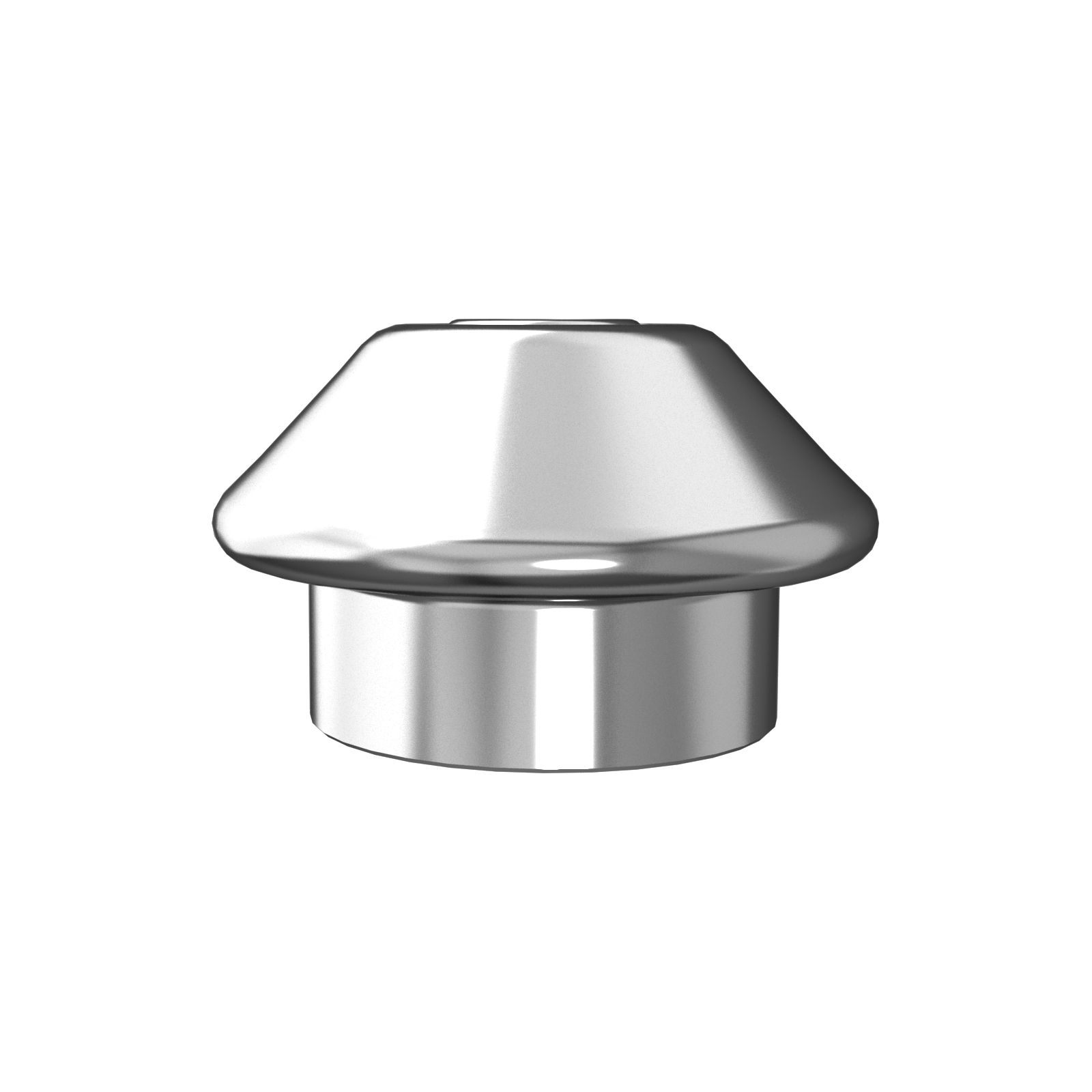
Placement of healing abutments and flap repositioning with suturing.
- Bone Regeneration Status at 6 Months Post-Op:
Radiographic and clinical evaluation confirmed satisfactory bone regeneration in the grafted area.

- Placement of Healing Abutments with Flap Repositioning and Suturing:
After uncovering the implants, healing abutments were installed, followed by careful flap adaptation and suturing.


- Postoperative View After Healing Abutment Placement:
Healing abutments were well seated, and soft tissue healing proceeded uneventfully.

Prosthetic Restoration:
Four weeks after healing abutment placement, the healing abutments were removed, and the final crowns were delivered.
4) Final crown placement completed.

POSTOPERATIVE FOLLOW-UP
Evaluation of osseointegration at 7 months postoperatively.

CLINICAL CHALLENGES
This case presents not only horizontal bone augmentation but also the aesthetic challenges associated with anterior maxillary implant restoration. One key clinical consideration is how to maintain stability given the limited bone height in the maxillary sinus area around tooth position 16.
- Adequate Tension Release During Surgery
Due to the loss of most posterior teeth in both jaws, the patient exhibited varying degrees of bone resorption and generally low bone density. The block bone grafting technique was chosen to utilize the barrier effect of the block to maintain space for osteogenesis and to enhance the osteoinductive potential of the grafted area. Given the relatively low bone density in the maxilla, excessive bone resorption during healing was a concern. To minimize the pressure from soft tissue and the risk of graft resorption, it was crucial to perform adequate tension release at the grafting site. - Long-term Maintenance of Periodontal Health
The patient presented with a thick gingival biotype, which reduced the need for gingival grafting. Adequate gingival thickness also contributes to forming a natural biological barrier around the implant, which is essential for long-term peri-implant health. However, achieving this outcome relies heavily on the clinician’s experience with aesthetic restorations. Long-term implant stability depends not only on the emergence profile of the crown but also on the ability of the soft tissue to close the interproximal space around the restoration. Therefore, flap rotation was performed to improve the soft tissue condition prior to final prosthetic restoration. - Low Bone Height in the Maxillary Sinus and Its Implication on Implant Placement
In this case, the bone height in the maxillary sinus area was as low as 6.62 mm. To ensure sufficient bone-to-implant contact for osseointegration, implants were inserted at an oblique angle. This approach allowed the use of appropriately long implants while preserving the necessary bone contact area. A bridge-type restoration was chosen to help stabilize implant positions. To minimize the risk of implant displacement into the sinus cavity, follow-up frequency during the healing period was increased compared to standard implant protocols.