With the continuous advancement of dental technology, dental implants have gradually become the mainstream solution for addressing tooth loss. By implanting artificial tooth roots into the jawbone, dental implants simulate the structure and function of natural teeth. They not only closely resemble natural teeth in appearance but also effectively restore chewing ability, significantly improving the patient’s quality of life. However, the debate surrounding whether dental implants are a “permanent” solution persists. Patients often wonder: Can dental implants last a lifetime like natural teeth? What factors influence their lifespan?
In fact, the “permanence” of dental implants does not mean indefinite, lifelong use, but rather long-term stability based on medical standards. International clinical data shows that, with proper procedure and maintenance, the 10-year survival rate of dental implants can exceed 95%, and some patients can use them for over 20 years. However, the lifespan of a dental implant is closely related to factors such as material choice, oral hygiene habits, overall health, and post-operative care. For example, titanium alloy implants, known for their excellent biocompatibility, have become the global standard; whereas insufficient bone volume or smoking habits can significantly shorten the implant’s lifespan.
This article will start by explaining the basic principles of dental implants, and, combined with clinical data and expert opinions, systematically analyze the factors that affect the lifespan of dental implants, daily maintenance tips, common causes of failure, and preventive strategies. This will help patients scientifically understand the “permanent” nature of dental implants and provide practical maintenance advice.
Advantages of Dental Implants
Long-Term Stability
As the ultimate solution for missing teeth, dental implants owe their core advantages to the integration of biomimetic principles and osseointegration technology. Titanium alloy implants, enhanced by surface treatment techniques such as sandblasting and acid etching or hydroxyapatite coatings, increase their biological activity and form a direct bone-to-bone connection (osseointegration) with the jawbone. This creates a mechanical system similar to natural tooth roots. Clinical studies show that the 5-year survival rate of properly placed implants exceeds 98%, and the 10-year survival rate is over 95%, with some cases maintaining lifelong function. This stability significantly outperforms traditional restorative options like dentures or fixed bridges, particularly in cases of multiple tooth loss or edentulous arches, where dental implants demonstrate even greater long-term advantages.
Function and Aesthetics Combined
Dental implants restore more than just the structure of the teeth; they rebuild the occlusal relationship (such as vertical distance and anterior guidance angle), recovering over 90% of chewing efficiency. This effectively prevents temporomandibular joint disorders (TMJ) and occlusal trauma caused by tooth loss. The restorative design (such as zirconia all-ceramic crowns) uses digital scanning and computer-aided design (CAD/CAM) technology to ensure precise fitting with neighboring teeth (marginal adaptation ≤ 50μm). This results in the restoration of natural gum contours and smile aesthetics. Patient satisfaction surveys show that oral health-related quality of life (OHRQoL) improves by 30%-50% post-implant, with a significant boost in social confidence.
Biological Effects of Osseointegration
The osseointegration mechanism of dental implants stimulates bone cell metabolism, maintaining the height and density of the alveolar bone (with an average annual bone resorption rate of < 0.2mm). It effectively counters the vertical and horizontal resorption of the alveolar ridge that often occurs after tooth loss. This effect is especially significant in immediate implant and immediate loading techniques, where the early stability of the implant and dynamic balance of occlusal forces promote bone regeneration and vascularization. Compared to traditional restoration methods, dental implants reduce the risk of alveolar ridge resorption by approximately 70%, providing a more stable foundation for future restorations (such as implant-supported dentures).
Comfort and Convenience
Dental implants can be placed using either “immediate implant—immediate restoration” or “delayed implant—immediate loading” techniques, allowing for fixed restorations right after surgery. This eliminates the need for daily removal and cleaning, completely removing the discomfort, baseplate pressure, and risk of mucosal ulcers associated with removable dentures. The digital implant navigation system (such as dynamic navigation or static templates) guides the placement of implants with sub-millimeter precision using 3D imaging, significantly reducing surgical trauma and post-operative swelling. Patient pain scores (VAS) are reduced by 60% compared to traditional surgeries, and the healing period is shortened to 3-6 months, providing long-term comfort that closely matches that of natural teeth.
Success Rate and Key Factors Affecting the Success of Dental Implants
1. Success Rate of Dental Implants
Success Rate Data:
The overall success rate of dental implants is typically over 95%, with some high-quality medical institutions achieving success rates as high as 98%-99%. This data reflects the maturity of dental implant technology, but the actual success rate can vary due to individual differences.
Sources of Success Rate Variations:
- Time Dimension: Short-term success rates (1-5 years) are usually higher, while long-term success rates (over 10 years) may decrease slightly due to factors like bone resorption and periodontal disease.
- Individual Differences: Factors such as the patient’s age, bone density, oral hygiene habits, and overall health can directly impact the success rate.
2. Key Factors Affecting the Success of Dental Implants
| Factor | Mechanism of Influence | Typical Cases |
|---|---|---|
| Bone Density | Insufficient bone mass can lead to poor initial stability of the implant, affecting osseointegration. | The upper posterior region, where bone quality is often poor, may require bone grafting; the lower anterior region tends to have better bone density, leading to higher success rates. |
| Gum Health | Gum diseases such as gingivitis or periodontitis may lead to peri-implantitis, causing implant loosening and failure. | Gum diseases should be thoroughly treated before surgery, and regular maintenance of gum health is essential post-surgery. |
| Smoking Habits | Nicotine inhibits bone cell activity, increases infection risk, and lowers success rates by approximately 10%-20%. | Smokers should quit at least 2 weeks before surgery, and continuing to smoke post-surgery may require more frequent follow-ups. |
| Overall Health | Conditions such as diabetes or osteoporosis may delay bone healing, while immune system disorders increase infection risk. | Diabetic patients should control blood sugar levels, and osteoporosis patients should supplement calcium. |
3. Strategies to Improve the Success Rate of Dental Implants
Pre-surgery Assessment:
- Comprehensive oral examination (CT scan, periodontal assessment)
- Full-body health screening (blood tests, coagulation function)
- Develop a personalized treatment plan
Intra-surgery Procedures:
- Choose an experienced implant specialist
- Strict sterile procedures to minimize infection risk
- Precise implantation angle and depth to ensure initial stability
Post-surgery Care:
- Apply cold compresses within 24 hours, avoid vigorous physical activity
- Follow prescribed antibiotics and painkillers
- Remove sutures 7-10 days post-surgery, avoid applying pressure to the implant site
Long-term Maintenance:
- Regular follow-ups (every 6 months)
- Professional dental cleanings (1-2 times a year)
- Prompt treatment of peri-implantitis
4. Special Case Handling Recommendations
- Immediate Implantation:
Suitable for sockets without infection, with success rates comparable to delayed implantation. However, strict adherence to indications is required. - Bone Augmentation Surgery:
When bone density is insufficient, techniques like Guided Bone Regeneration (GBR) or sinus lift surgeries are used to increase bone volume, with a success rate of approximately 90%. - Full Arch Edentulous Implantation:
Using the All-on-4/6 technique, implants are tilted to achieve fixed restorations, with a success rate of about 95%.
Are Dental Implants Permanent?
1. Durability and Lifespan of Dental Implants
Dental implants are not “permanent” in the traditional sense, but their lifespan typically exceeds 20 years, with some patients even able to use them for a lifetime. The expected lifespan of an implant is influenced by several factors:
- Implant Material:
Biocompatible materials, such as titanium alloys, form stable bonds with bone tissue, extending the implant’s lifespan. - Oral Care:
Inadequate daily cleaning can lead to peri-implantitis, affecting long-term stability. - Overall Health:
Conditions like diabetes and osteoporosis may delay bone healing, reducing the implant’s lifespan.
2. Comparison with Other Restoration Methods
| Restoration Method | Advantages | Disadvantages | Lifespan |
|---|---|---|---|
| Dental Implants | Stable, durable, and close to natural tooth function | High initial cost, requires surgery | 20+ years |
| Traditional Dentures | Lower cost, wide adaptability | Requires replacement every 3-5 years, prone to wear | 3-8 years (requires replacement) |
| Fixed Bridges | No surgery required, aesthetically pleasing | Requires grinding of adjacent teeth, limited adaptability | 10-15 years |
3. Key Measures to Extend the Lifespan of Dental Implants
- Oral Hygiene Maintenance:
- Use a soft-bristled toothbrush, dental floss, and special cleaning tools for implants daily.
- Schedule professional cleanings regularly (recommended every 6 months).
- Lifestyle Adjustments:
- Quit smoking and limit alcohol intake, as nicotine inhibits bone cell activity.
- Avoid chewing hard objects to prevent mechanical damage to the implant.
- Regular Checkups:
- Follow up every 3 months during the first year after surgery, then every 6-12 months to check implant stability.
- Address issues such as peri-implantitis or abutment loosening promptly.
- Overall Health Management:
- Control blood sugar and blood pressure to reduce infection risk.
- Osteoporosis patients should follow medical advice to supplement calcium and vitamin D.
4. Special Considerations in Certain Cases
- Immediate Implantation:
Requires strict sterile techniques, and patients should avoid strenuous activity post-surgery. Initial stability may be slightly lower than delayed implantation. - Full Arch Edentulous Implantation:
When using All-on-4/6 techniques, it is important to maintain occlusal balance and avoid excessive pressure on one side. - Patients with Periodontal Disease:
Thorough treatment of periodontal disease should be completed before surgery, and regular follow-ups should be scheduled to monitor gum health after surgery.
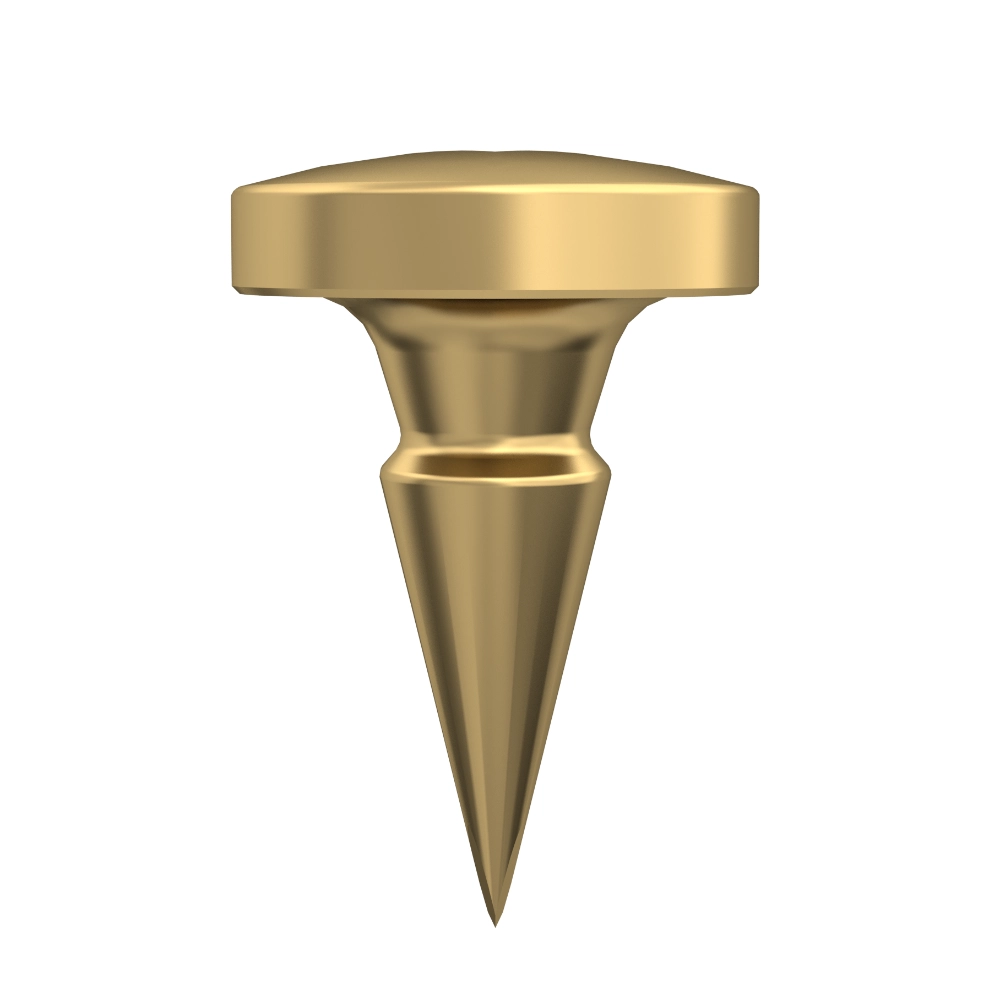
Structure of a Dental Implant
As the “gold standard” in modern dental restoration, the structure of a dental implant is ingeniously designed to replicate the chewing function, aesthetics, and long-term stability of natural teeth. From a professional standpoint, the implant system consists of three core components:
1. Implant
Definition:
A metal screw surgically inserted into the jawbone, acting as an “artificial tooth root” that provides biomechanical support for the entire restoration.
Key Features:
- Material:
Medical-grade pure titanium (Grade IV) or titanium alloy, known for excellent biocompatibility, enabling osseointegration (the direct bond between implant and bone tissue). - Surface Treatment:
Techniques like sandblasting, acid-etching, or laser microstructuring increase the surface area and promote bone cell attachment and integration. - Shape Design:
- Root-form implants: Mimic natural tooth roots, suitable for most standard cases.
- Cylindrical implants: Used in cases with limited bone volume or immediate implantation.
- Tapered implants: Ideal for immediate loading or use in the aesthetic zone.
Clinical Significance:
The success of the implant depends on the quality of osseointegration. Preoperative imaging (e.g., CBCT scans) is used to evaluate bone density, volume, and implant stability.
2. Abutment
Definition:
The intermediate connector between the implant and the prosthesis, responsible for transmitting chewing forces and adjusting the position and angle of the final restoration.
Key Features:
- Material:
Titanium alloy, zirconia, or custom-made (via CAD/CAM technology). - Types of Abutments:
- Prefabricated abutments: Standardized designs for most cases.
- Custom abutments: Tailored to match gingival contours for optimal aesthetic results.
- Angled abutments: Compensate for implant angle discrepancies and help prevent gum recession.
- Functions:
- Soft tissue seal: Forms a biological seal with the gum to block bacterial invasion.
- Stress distribution: Anti-rotation design minimizes micromovement and stress on the implant.
Clinical Significance:
Abutment selection directly impacts the fit of the prosthesis and the surrounding soft tissue aesthetics. Customization based on gingival biotype (thick vs. thin tissue) is crucial for optimal outcomes.
3. Prosthesis (Crown, Bridge, or Denture)
Definition:
The visible artificial tooth (or teeth) attached to the abutment, restoring both chewing function and aesthetics.
Key Features:
- Material Options:
- All-ceramic prosthetics: Zirconia, glass ceramics (e.g., IPS e.max) – ideal for the aesthetic zone.
- Porcelain-fused-to-metal (PFM): Noble metals (e.g., gold alloy) or base metals (e.g., cobalt-chromium) – ideal for posterior teeth.
- Attachment Methods:
- Screw-retained: Secured through a screw hole in the abutment; allows for easier maintenance.
- Cement-retained: Bonded using resin cement – preferred in highly aesthetic cases.
- Design Types:
- Single crown: For individual missing teeth.
- Bridge: For multiple adjacent missing teeth.
- Overdenture: Implant-supported removable dentures for edentulous (toothless) arches.
Clinical Significance:
Prosthetic design must balance functional load (e.g., chewing forces in posterior regions) with aesthetic requirements (e.g., translucency and color matching in the front teeth).
Clinical Synergy of the Implant Structure
- Biomechanical Stability:
The implant–abutment–prosthesis complex forms a stress-buffering system, reducing micromovement and bone resorption. - Soft Tissue Aesthetics:
A well-designed abutment and prosthesis can simulate natural gingival papillae and create a lifelike emergence profile. - Long-Term Maintenance:
The modular design (with removable implant, abutment, and prosthesis components) allows for convenient cleaning, monitoring, and repairs over time.
Material Selection for Dental Implants
In the field of dental implant restoration, the choice of implant material is one of the key factors determining the success, longevity, and overall user experience of the implant. Among the various materials available, high-quality titanium alloys have become the most commonly used due to their unique advantages.
Titanium alloys offer exceptional biocompatibility. When implanted into the jawbone, the human body exhibits minimal rejection responses. This is primarily because a dense oxide layer naturally forms on the surface of titanium, effectively preventing the release of metal ions into the surrounding tissues. This protective layer acts like a “shield,” reducing the risk of allergic reactions, inflammation, and other adverse effects. It enables the implant to coexist harmoniously with the human body, laying a solid foundation for long-term stability.
In terms of strength, titanium alloys perform exceptionally well. The oral environment is dynamic and complex, constantly subjected to forces from chewing and biting. High-quality titanium alloys possess both high strength and excellent toughness, allowing them to withstand significant occlusal forces without fracturing or deforming. Like a resilient “guardian,” titanium provides unwavering support, ensuring that the dental implant functions like a natural tooth and meets the patient’s everyday dietary needs.
Thanks to the combination of biocompatibility and mechanical strength, titanium alloys ensure both the stability and durability of dental implants. After placement, they form a strong osseointegrated bond with the surrounding jawbone, anchoring the implant as firmly as a natural tooth root. This solid integration not only guarantees a secure fit during use but also significantly extends the lifespan of the implant, offering long-term benefits to the patient.
As dental technology continues to evolve, many new implant materials have emerged. However, high-quality titanium alloys remain an irreplaceable standard in the field due to their long-standing clinical success and reliability. They continue to provide countless patients with healthy, aesthetically pleasing, and long-lasting implant restorations.
Potential Causes of Dental Implant Failure
Poor Oral Hygiene — Inadequate Post-Operative Care
Maintaining good oral hygiene after implant surgery is critical. However, some patients fail to give it the necessary attention. Improper brushing techniques and incorrect flossing habits allow plaque to accumulate around the implant site. Plaque, often called an “invisible killer,” gradually hardens into tartar, which irritates the gum tissue and triggers inflammation. As the condition worsens, bacteria may infiltrate the area where the implant integrates with the surrounding bone, compromising osseointegration and causing infection. This process can ultimately lead to implant failure.
Insufficient Bone Volume — Hindering Implant Stability
Successful dental implantation relies heavily on solid osseointegration, which requires sufficient bone volume. For patients lacking adequate bone mass, the implant is like a seed planted in shallow soil — it struggles to establish a firm hold. When subjected to forces from chewing, the implant may loosen and fail to bond tightly with the surrounding bone tissue. This compromises both functionality and increases the risk of failure. In such cases, bone grafting becomes essential. By using autogenous bone, allografts, or synthetic bone materials, bone volume can be restored to provide a solid foundation for the implant.
Smoking and Other Harmful Habits — The Effects of Smoking
Smoking has a notably negative impact on implant healing and stability. Harmful substances in tobacco constrict blood vessels in the gums, reducing blood flow and impairing nutrient delivery to the tissues around the implant. Additionally, smoking weakens the immune system, lowers resistance to infection, and slows down the healing process. Poor healing leads to inadequate bonding between the implant and bone, significantly increasing the risk of failure.
Bruxism — The Impact of Teeth Grinding on Implants
Bruxism, or teeth grinding, is a harmful oral habit and poses a serious risk for dental implant patients. The excessive bite force generated during grinding directly affects the implant. Over time, this unnatural stress can damage the implant’s structural components, causing it to loosen or even fracture. Bruxism can also lead to bone resorption around the implant, further jeopardizing its stability.
Other Factors — Diabetes, Medications, and More
Certain health conditions and medications can also affect implant healing and stability. For example, patients with poorly controlled diabetes may have weakened immune responses and delayed wound healing, raising the likelihood of infection and implant failure. Long-term use of certain medications such as immunosuppressants or corticosteroids may interfere with bone metabolism and immune function, impeding the integration between the implant and bone, and increasing the risk of failure.
Treatment Options for Failed Dental Implants
When a dental implant fails, prompt and effective intervention is crucial. Typically, the failed implant must first be removed to prevent further damage to surrounding tissues. This removal may result in some bone loss at the implant site, making bone reconstruction procedures — such as bone grafting — necessary to restore a suitable foundation for future implantation. Once healing is complete and sufficient bone has been regenerated, a new implant can be placed at the optimal time, ensuring adequate support to minimize the chances of another failure.
How to Prevent Implant Failure
Preventing dental implant failure requires a comprehensive approach. Choosing a skilled and experienced dental professional is essential, as they can tailor treatment plans to suit individual patient needs and maximize surgical success. Post-operatively, patients must follow all care instructions closely, including proper oral hygiene and a well-balanced diet. Regular dental check-ups are also vital; with professional monitoring, any early warning signs can be detected and addressed promptly, ensuring the long-term stability and functionality of the implant.