Although dental implants are designed to last for several decades, they are not permanent. Clinical studies have shown that with proper care, 90-95% of dental implants can last for over 10 years.
Understanding Dental Implant Longevity
When discussing oral health, dental implants are a cutting-edge dental restoration technique, and their lifespan is a major concern for patients. Understanding the true meaning of “permanent” and the differences in lifespan between dental implants and other dental restoration methods is essential for making informed decisions.
The True Meaning of “Permanent”
In dentistry, the term “permanent” does not equate to indefinite or eternal. For dental implants, it refers more to a long-term stable solution aimed at replicating the function and appearance of natural teeth. Dental implants form a biological foundation by integrating with the jawbone (osseointegration) to provide firm support. However, this does not mean that implants are immune to the passage of time or require no maintenance.
There is a distinction between the implant itself and the crown. The implant, if properly placed and well-maintained, can last for decades. On the other hand, the crown, the artificial tooth placed on the implant, may need to be replaced due to wear, aging, or technological advancements. Therefore, when discussing the lifespan of dental implants, it is important to view the implant and the crown as two independent but interconnected components.
Clinical Survival Rate
Clinical studies show that with proper care, the 10-year survival rate of dental implants can reach as high as 90-95%. This means that, in most cases, dental implants provide long-term stable restoration. However, survival rates are influenced by several factors, including the patient’s oral health condition, the skill level of the implant surgery, and postoperative maintenance.
In addition to short-term survival data, long-term case studies provide deeper insights into the lifespan of dental implants. Historical data from organizations like ASIRD (American Society of Implant Dentistry) show that some dental implants continue to function well even 30 years after placement. These cases suggest that dental implants can potentially be a lifelong dental restoration solution for patients.
Comparison Chart: Dental Implants, Bridges, and Dentures
To better understand the lifespan advantages of dental implants, we can compare them with other common dental restoration methods. Below is a simplified comparison chart:
| Dental Restoration Method | Average Lifespan (Years) | Maintenance Requirements |
|---|---|---|
| Dental Implants | Several decades (or longer) | Regular checkups and cleaning |
| Dental Bridges | 5-15 years | Requires regular checkups and possible repairs or replacement |
| Dentures | 5-10 years (removable); longer (fixed) | Requires regular adjustments or replacement; removable dentures need daily cleaning and maintenance |
From the chart, it is evident that dental implants typically outlast other dental restoration methods. However, this does not mean that implants are the best choice for everyone. When choosing a dental restoration option, patients should consider factors such as their oral health, financial situation, and personal preferences. Regardless of the restoration method, regular oral checkups and maintenance are essential for maintaining good oral health.
Key Factors Determining Implant Lifespan
The lifespan of dental implants is influenced by a variety of factors, which can be broadly categorized into surgical factors, patient-related factors, and maintenance factors. Understanding these factors helps us better predict and maintain the long-term effectiveness of dental implants.
Surgical Factors
Board-Certified Surgeon Expertise
The success of the surgery largely depends on the experience and skill of the surgeon. Board-certified surgeons typically possess more extensive expertise and a higher level of technical proficiency, enabling them to assess the patient’s oral condition more accurately, develop an appropriate surgical plan, and take necessary preventive measures during the procedure. This reduces surgical risks and increases the survival rate of dental implants.
Bone Density Requirements
Bone density is one of the crucial factors influencing the success of dental implants. Sufficient bone density provides stable support, ensuring good integration between the implant and the jawbone. If bone density is insufficient, bone augmentation procedures may be necessary to increase bone volume, thereby enhancing the stability of the implant.
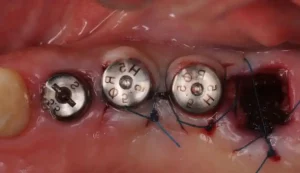
Correct Placement Technique
The placement position, depth, and angle of the implant are critical for the success of the dental implant. Correct placement ensures good contact between the implant and surrounding tissues, reduces complications, and improves the survival rate and long-term stability of the implant.
Patient-Related Factors
Oral Hygiene Habits
Oral hygiene habits are key factors in determining the lifespan of dental implants. Good oral hygiene can reduce the number of bacteria in the mouth, lower the risk of infection, and protect the implant and surrounding tissues. Patients should develop regular brushing, flossing, and mouthwash habits.
Smoking/Tobacco Use (Risk of Failure is 3 Times Higher)
Smoking and tobacco use negatively affect the success rate of dental implants. Research shows that the risk of implant failure is about three times higher in smokers compared to non-smokers. Harmful substances in tobacco damage the oral mucosa and bone, reduce implant stability, and increase the risk of infection.
Medical Conditions: Diabetes, Osteoporosis
Certain medical conditions, such as diabetes and osteoporosis, can also affect the success rate of dental implants. Diabetic patients, due to poor blood sugar control, are more prone to infections and poor tissue healing, while osteoporosis patients may not provide enough support due to bone loss. Therefore, patients should undergo a thorough physical examination before implant surgery to assess potential risks.
Maintenance Factors
Importance of Professional Cleaning
Regular professional cleaning at dental clinics is an essential measure to maintain the health of dental implants. Professional cleaning thoroughly removes plaque and calculus from the tooth surface, reducing the risk of infection and protecting the implant and surrounding tissues.
Night Guard for Bruxism Patients
Bruxism patients, who unconsciously grind their teeth at night, may place additional stress on the implant, increasing the risk of failure. Therefore, bruxism patients should wear a night guard to reduce damage to the implant.
Crown Replacement Cycle (Every 15-20 Years)
The crown, as the artificial tooth on the implant, may need to be replaced due to wear, aging, or technological advancements. Generally, the replacement cycle for crowns is around 15-20 years. Regular checkups and timely replacement of worn-out crowns can extend the lifespan of the dental implant.
In conclusion, the key factors determining the lifespan of dental implants include surgical factors, patient-related factors, and maintenance factors. Understanding these factors and taking appropriate preventive and maintenance measures can help us better protect the health of dental implants and extend their lifespan.
Warning Signs of Potential Failure
While dental implants are a long-term and stable solution for tooth restoration, they can still face the risk of failure. Understanding the potential warning signs of failure helps us identify and take necessary actions to protect the health of the implant. Below are the early warning signs and long-term risks associated with implant failure.
Early Stage Red Flags
Symptoms of Infection (Peri-implantitis)
Peri-implantitis is one of the most common early warning signs of implant failure. It typically manifests as redness, swelling, pain, and bleeding around the implant area. If left untreated, the infection may spread, causing bone loss and implant loosening.
Loosening Sensation
Under normal circumstances, the implant should be tightly integrated with the jawbone, providing stable support. If a patient feels the implant loosen when chewing or touching, this could be a sign that the implant has not properly integrated with the bone. It is essential to seek immediate medical attention for an evaluation.
Gum Recession Around the Implant
Gum recession is another early warning sign of implant failure. It is characterized by the gum tissue around the implant shrinking, exposing more of the implant surface. Gum recession may lead to the implant being exposed to the oral environment, increasing the risk of infection.
Long-term Risks
Progressive Bone Loss
Over time, the bone surrounding the implant may gradually deteriorate. This could be due to the implant failing to form a stable bond with the jawbone, or because of poor oral health conditions in the patient. Bone loss may result in decreased implant stability, increasing the risk of failure.
Wear and Tear of Mechanical Components
Mechanical components in dental implants, such as crowns, abutments, and screws, may develop issues due to long-term use and wear. For example, the crown may need to be replaced due to wear or aging, and the abutment or screws might loosen or break. The wear and tear of these mechanical parts can affect the implant’s function and appearance.
Changes in Bite Force with Age
As patients age, their bite force may change. This can be caused by tooth wear, gum disease, or other oral health issues. Changes in bite force may put additional pressure on the dental implant, increasing the risk of failure. Therefore, patients should regularly visit dental clinics for checkups and adjustments to ensure the implant’s stability and function.
Prolonging Your Implant’s Lifespan
To ensure the long-term stability and functionality of dental implants, it is crucial to adopt a series of effective maintenance and care measures. Below are recommendations for daily cleaning routines, the frequency of 3D imaging checks, and dietary adjustments to help extend the lifespan of implants.
5-step daily cleaning routine
- Brushing: Brush your teeth at least twice a day using a soft-bristled toothbrush and mild toothpaste. Pay special attention to the implant and the surrounding gum area to thoroughly remove plaque and food debris.
- Flossing: Flossing is important for cleaning the gaps between implants. Use specialized dental floss or interdental brushes to gently pass through the spaces between the implants, removing hard-to-reach food particles and plaque.
- Importance of Interdental Brushes: Interdental brushes are particularly effective for cleaning tight spaces between implants and adjacent teeth. They can reach these difficult areas, effectively removing plaque and food debris, preventing gum inflammation and bone loss.
- Mouthwash: Use fluoride mouthwash to strengthen teeth against cavities and reduce the number of bacteria in the mouth. It’s recommended to use mouthwash at least once a day, especially after brushing.
- Regular Professional Cleaning: In addition to daily cleaning, patients should regularly visit a dental clinic for professional cleaning. Professional cleaning can thoroughly remove plaque and tartar, helping to protect the health of the implants and surrounding tissues.
3D imaging checkup frequency
3D imaging technologies, such as Cone Beam CT (CBCT), provide detailed images of the implant and surrounding tissues. This helps dentists assess the stability and health of the implants, and detect and address potential problems early. It is recommended that patients undergo regular 3D imaging checks (e.g., once a year) after dental implant surgery to ensure the long-term stability of the implant.
Diet modifications (avoiding ice/hard candy)
Diet also plays an important role in the lifespan of dental implants. To avoid unnecessary pressure or damage to the implants, patients should follow these dietary recommendations:
- Avoid eating foods that are too hard, sticky, or overly spicy, such as ice cubes, hard candies, nuts, etc. These foods may cause implants to loosen or get damaged.
- Choose soft and easily digestible foods to reduce wear and pressure on the implants.
- Increase intake of calcium and vitamin D-rich foods, such as dairy products, fish, and leafy vegetables, to promote bone health.
In summary, by following the five daily cleaning steps, regularly undergoing 3D imaging checks, and adjusting dietary habits, patients can effectively extend the lifespan of their implants, maintaining both oral health and aesthetics.
Technological Advancements in Dental Implants
Technological advancements in the field of dental implants have provided patients with more and better treatment options. Zirconia implants, antimicrobial coatings, guided bone regeneration (GBR) technology, and AI implant planning are key research directions and technological trends in the field of dental implants. These continuous innovations and developments will help improve the success rate and lifespan of implants, providing patients with better treatment outcomes and experiences.
1. Advances in Zirconia Implant Research
Zirconia, as a new type of dental implant material, has garnered widespread attention and research in recent years. Compared to traditional titanium implants, zirconia implants offer better biocompatibility, aesthetics, and durability. Studies have shown that zirconia implants can reduce inflammation and bone resorption around the surrounding tissues after implantation, while also providing good aesthetic results. Additionally, zirconia implants have lower surface energy and wettability, which helps reduce plaque adhesion. However, zirconia implants have not shown significant advantages in terms of bone induction ability compared to titanium, and their fracture strength and wear resistance still need further research and improvement. Currently, zirconia implants are widely used in clinical practice and have achieved good treatment results.
2. Innovations in Antimicrobial Coatings
The application of antimicrobial coatings in dental implants is becoming increasingly widespread. By spraying antimicrobial coatings on the surface of implants, bacterial adhesion and proliferation on the implant surface can be effectively reduced, thereby lowering the risk of infection. Ultrasonic spraying technology is an advanced coating preparation process with advantages such as high coating uniformity, high material utilization, precise control of coating thickness, and environmental and economic benefits. Antimicrobial coatings prepared by ultrasonic spraying can form a durable and effective antimicrobial barrier, protecting the implant and surrounding tissues. In the future, as antimicrobial coating technology continues to innovate and develop, its application prospects in dental implants will be even broader.
3. Guided Bone Regeneration (GBR) Technology
Guided Bone Regeneration (GBR) is a commonly used bone augmentation technique that has broad applications in the field of dental implants. This technology involves placing a barrier membrane between the soft tissue and bone defect, creating a biological barrier that prevents connective tissue cells and epithelial cells from entering the bone defect area. This allows precursor osteoblasts, which have slower migration speeds and potential growth ability, to enter the bone defect area for growth and repair. GBR technology is mainly used to address horizontal and vertical bone deficiencies in the alveolar ridge, as well as bone deficiencies in immediate or early implant placements. Through GBR technology, patients can achieve bone augmentation in the implant area, which enhances the stability and success rate of implants.
4. AI Implant Planning Technology Trends
With the continuous development of artificial intelligence (AI) technology, AI implant planning has become a major trend in the field of dental implants. AI technology can provide accurate implant planning information, such as implant position, depth, and angle, by comprehensively analyzing and assessing the patient’s oral condition. This not only helps the surgeon place the implant more accurately during surgery but also reduces surgical time and trauma, improving patient comfort and satisfaction. Moreover, AI technology can offer personalized treatment plans and prognosis evaluations based on the specific conditions and needs of the patient. In the future, as AI technology continues to advance and be applied, its role in dental implants will become even more prominent.
When Might Replacement Be Needed?
Dental implants are generally a long-term and stable solution for tooth restoration, with most implants lasting for many years. However, there are certain circumstances in which an implant may need to be replaced. Below are some common situations that may require implant replacement, along with a cost-benefit analysis.
Common Situations
- Trauma/Accidental Damage: If a dental implant is damaged due to external forces (such as a car accident, fall, or impact), it could cause the implant to become loose, fractured, or result in surrounding bone damage. In such cases, the implant may need to be replaced or repaired.
- Late Bone Resorption: Although implants typically integrate well with the jawbone after placement, conditions like osteoporosis or peri-implantitis can lead to gradual bone loss around the implant. When bone resorption reaches a certain point, the implant may no longer provide sufficient support, necessitating a replacement.
- Fracture of Prosthetic Components: The components of a dental implant system, such as the crown, abutment, or screw, may fracture over time due to prolonged use, wear, or quality issues. In such cases, the damaged components or the entire implant system may need to be replaced.
Cost-Benefit Analysis
- Average Replacement Cost Compared to a New Implant: The cost of replacing a dental implant typically includes surgical fees, material costs, and post-surgical recovery expenses. The cost of implant replacement may vary due to factors like the type and brand of the implant, the difficulty of the surgery, and regional price differences. However, in most cases, the cost of replacing an implant is comparable to or sometimes even higher than the initial cost of implantation.
- Insurance Coverage Considerations: Dental implants are often considered a cosmetic procedure, so most basic medical insurance plans may not cover their cost. However, in some cases, such as when an implant is damaged due to an accident, certain medical insurance plans may offer reimbursement. It’s essential for patients to consult with their insurance company or healthcare provider to understand the specific insurance coverage and reimbursement policies related to implant replacement.
- Age-Related Surgical Risk Assessment: As patients age, their overall health and surgical tolerance may decline. When undergoing an implant replacement surgery, doctors need to conduct a thorough assessment of the patient’s age, health status, and potential surgical risks. For elderly patients, more conservative treatment approaches may be recommended, such as localized repairs or alternative treatment options to minimize risks and ensure the best possible outcome.
FAQ Section
Do dental implants last forever?
Dental implants do not guarantee eternal use. Although some reports indicate that implants can last up to 50 years or more, this is not the case for everyone. The lifespan of a dental implant depends on various factors, including the expertise of the dentist, the patient’s self-care and maintenance, oral hygiene habits, gum and bone health, and overall health. While implants may theoretically last forever, the actual duration varies from person to person.
How often do implants need maintenance?
Implants generally require maintenance every 3 to 6 months. The exact frequency depends on the individual’s oral condition. If the patient’s oral health is not optimal, more frequent maintenance (about every 3 months) may be necessary. However, if the patient maintains good oral hygiene, a check-up every 6 months is usually sufficient. Regular dental check-ups and proper oral care are essential to maintaining the longevity of dental implants.
Can failed implants be replaced?
Yes, failed implants can be replaced. If an implant fails, it will be removed, and once the surrounding tissues heal and the bone is healthy again, a new implant can be placed. The process requires a skilled dentist to ensure a high success rate for the procedure and the stability of the new implant.
What’s the oldest dental implant still functioning?
The oldest functional dental implants depend on several factors, such as the materials used, the patient’s oral care, and the implant’s maintenance. If a dental implant has undergone long-term clinical trials and the patient maintains good oral hygiene with slow bone resorption, it can continue to function well even after many years. However, not all long-term implants remain functional, so regular check-ups and maintenance are crucial for their ongoing success.
How long do permanent dental implants last?
“Permanent” dental implants are not truly permanent, as their longevity is affected by several factors. On average, implants can last about 20 years, with well-maintained implants potentially lasting 25 to 30 years, particularly those of higher quality. However, some patients may only experience around 15 years of service if they neglect oral care. Proper maintenance and good oral hygiene can significantly extend the lifespan of implants.
Can we implant teeth permanently?
As mentioned, “permanent” dental implants are not truly permanent. The use of implants is long-term and stable, but the duration varies based on maintenance, the implant material, and the patient’s oral health. While implants can offer a lasting solution for tooth restoration, they are not guaranteed to last forever.
Are full dental implants permanent?
Full dental implants are also not permanent. Their lifespan depends on factors like the material used, the dentist’s skill, the patient’s oral hygiene habits, and lifestyle. Although full-arch implants provide improved chewing function and aesthetic results, they still require ongoing care and regular dental visits to ensure their stability and longevity.
Is a permanent tooth implant painful?
Dental implant surgery may involve some discomfort, but it is generally manageable. Local anesthesia is used to minimize pain during the procedure. After the procedure, mild swelling and discomfort are common but typically resolve within a few days. Proper oral hygiene and avoiding foods that could damage the implant area will help speed up recovery. The pain is usually mild and temporary, with most patients experiencing little discomfort after the healing period.