Bone grafting is an essential therapy method in oral medicine, especially in dentistry, where it is used to restore dental functioning, aesthetics, and oral health. The techniques and supplies used for bone grafting have consistently improved due to developments in medical technology, giving patients more options and better results.
In contemporary dentistry, bone grafting is essential for treating patients whose bone density is too low to support dental implants or other restorative operations. Professionals and patients may make better selections if they are aware of the many kinds of bone transplants that are available. The primary kinds of bone grafts, their advantages, and how they support effective dental procedures are all covered in this blog.
Why Is Bone Grafting Needed in Dentistry?
Bone grafting is performed to replace lost bone due to:
- One major problem that causes bone degradation is periodontal disease.
- Tooth Loss: Over time, the surrounding bone may reabsorb as a consequence of missing teeth.
- Trauma: Bone structures may be harmed by injuries.
- Dental Implant Preparation: To firmly attach implants, there must be sufficient bone density.
- Grafting provides long-term stability for dental operations by increasing or rebuilding bone volume.
Types of Bone Grafts
- Autogenous Bone Grafts, or autografts
- Xenografts and Allografts
- Alloplasts
- Grafts in Composite
Advantages and Disadvantages of Each Bone Graft Type
- Autografts (Autogenous Bone Grafts): These procedures use patient bone, often taken from the hip, chin, or jaw.
Benefits: Provides living cells for osteogenesis, or the spontaneous rebuilding of bone.
Immune rejection is not a possibility.
Cons: Necessitates a second surgical site.
may lengthen the healing period and cause more pain. - The source of allografts is human bone tissue that has been safely processed and sterilized.
Advantages: No need for a secondary surgical site.
Large amounts are readily accessible.
Cons: Depends on osteoconductive and osteoinductive qualities; lacks living cells.
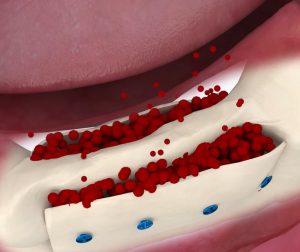
Despite thorough processing, there remains a slight chance of disease transmission. - The source of xenografts is animal bone, usually from pigs or cows.
Benefits: Outstanding scaffolding for osteoconduction, the formation of new bone.
Plenty and readily available.
Lack of osteogenic or osteoinductive qualities is a drawback.
Integrating into normal bone might take longer. - Synthetic materials like calcium phosphate, hydroxyapatite, or bioactive glass are the source of alloplasts.
Benefits include biocompatibility and adaptability for a range of uses.
limitless supply with no chance of disease transmission.
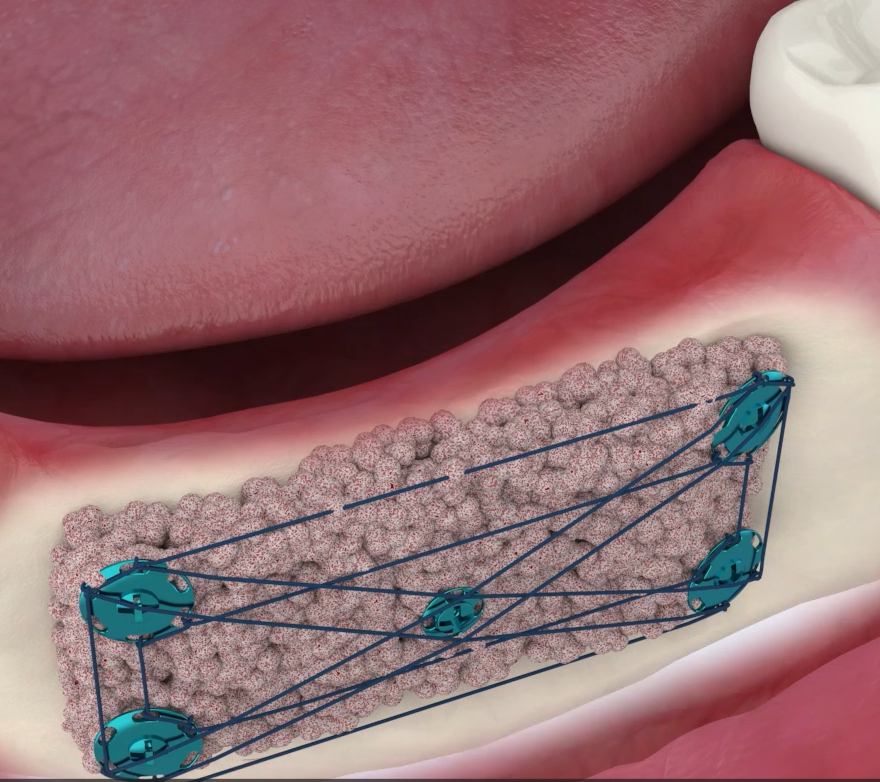
Cons: Less natural integration than organic alternatives. - Source for Composite Grafts: A mix of two or more transplant types, including allografts and autografts.
Benefits: Blends the best qualities of many graft varieties.
customized to fulfill certain patient requirements.
Cons: A more difficult application and preparation procedure.
How to Choose the Right Bone Graft Selection depends on several factors:
The selection of the appropriate bone grafting method depends on several factors, including the extent of bone loss, the patient’s health condition, surgical objectives, cost, and availability. Here’s a detailed analysis of these factors:
1. Extent of Bone Loss
- Mild Bone Loss: For patients with mild bone loss, autografts may be the preferred option. Autografts offer osteoconduction, osteogenesis, and osteoinduction properties, providing long-term stable repair outcomes.
- Severe Bone Loss: In cases of significant bone loss, xenografts or allografts may need to be considered. These methods can supply sufficient bone volume to fill defects. However, it is important to note that allografts carry risks of absorption and rejection.
2. Patient Health
- Suitability of Autografts: Autografts are generally suitable for patients in good health. However, for those with specific conditions (e.g., hematological disorders, immune system diseases), autografts may not be the best choice, as such conditions could affect bone regeneration and post-graft integration.
- Consideration for Allografts: For patients who cannot tolerate autografts, allografts may be a viable alternative. Preoperative evaluations and preparation are essential to reduce the risk of rejection and absorption.
3. Surgical Objectives
- Advantages of Composite Grafting: Composite grafting (e.g., vascularized bone grafting) offers faster integration and higher precision. This method not only provides sufficient bone volume but also retains blood supply to the graft, accelerating bone regeneration and repair.
- Choosing Based on Objectives: The choice of grafting method should align with the surgical goals. For patients requiring rapid functional recovery, composite grafting may be ideal. For those with lower functional demands, simpler grafting methods may suffice.
4. Cost and Availability
- Cost of Autografts: Autografts are typically more cost-effective, as they do not require additional donor materials. However, they may involve more complex surgical procedures and longer recovery times.
- Cost of Allografts: The cost of allografts can vary depending on the procurement, processing, and storage of donor materials. Compared to autografts, allografts often offer broader applicability and shorter recovery times.
- Consideration for Xenografts: While xenografts might be a more affordable option, their use is still relatively limited due to higher risks of rejection and potential disease transmission.
The Bone Grafting Procedure: What to Expect
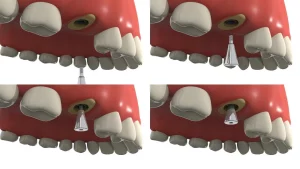
- Consultation: A dentist evaluates bone density and selects the appropriate graft type.
- The graft material is positioned at the treatment location during the surgical procedure.
- Healing Time: Over a few months, the graft fuses with the surrounding bone.
- Follow-Up: Routine examinations guarantee a smooth integration and get ready for the next procedures, such as implant implantation.
Uses for Bone Grafting
Bone grafting has extensive applications in dentistry, including:
- Increasing the amount of bone to support dental implants is known as bone augmentation.
- Restoring bone health to lower the risk of tooth loss is the treatment for periodontal disease.
- Rebuilding bone structure after traumas is known as maxillofacial trauma repair.
- Correcting Congenital Deformities: Dealing with anomalies of the jawbone during development.
Technological Developments in Bone Grafting
The materials and methods used in bone grafting have advanced significantly in modern dentistry. Accuracy and results are being improved by innovations including computer-guided surgery, bioactive graft materials, and 3D imaging.
Final Thoughts
Dental bone grafting is a difficult but necessary procedure that requires skill and accuracy. Due to the continuous advancement of medical innovation and technology, bone grafting continues to evolve, providing patients with more options and better results. However, all procedures are subject to potential dangers and side effects. Under the guidance of the dentist, patients should make an informed choice after thoroughly understanding the procedure, risks, and expected results.
To ensure a full recovery and achieve the best results, postoperative care and follow-up are equally important. Through the cooperation of patients and dentists, dental health and quality of life can be restored. For dentists, bone grafting instruments are also very important because they are related to the success rate and efficiency of the procedure.