Since the advent of dental implant technology in 1965, this innovation has benefited millions of patients worldwide, not only transforming their smiles but also significantly enhancing their quality of life. Dental implants, as an excellent solution for missing teeth, are surgically placed into the jawbone to mimic the structure of natural tooth roots, thereby providing stable support for restorations such as crowns, bridges, or dentures. This treatment restores both the function and aesthetics of the mouth, greatly improving chewing efficiency and boosting patients’ confidence, allowing them to navigate daily life with greater ease and self-assurance.
In the design and application of dental implants, the choice of material plays a crucial role, directly impacting the long-term effectiveness and longevity of the implants once they are successfully placed. Ideal implant materials must exhibit exceptional biocompatibility, meaning they can seamlessly integrate with bone tissue to facilitate the bonding process and ensure a stable support base. Additionally, these materials need to possess sufficient mechanical strength and durability to withstand the various forces and challenges posed by daily chewing activities, ensuring the long-term stability of the implants. Therefore, material selection is not only a consideration of technical precision but also a critical factor in ensuring patient comfort and treatment outcomes.

The Most Common Types of Dental Implant Materials
The field of dental implants has undergone significant evolution, traditionally relying on titanium and its alloys, which are renowned for their exceptional biocompatibility, durability, and ability to promote osseointegration, providing a stable and reliable foundation for tooth replacement. However, with technological advancements and progress in materials science, the range of materials for dental implants has expanded. Among these, biocompatible ceramics such as zirconia have emerged, demonstrating characteristics similar to titanium. Notably, in 2024, DentalMaster introduced an innovative titanium-zirconium alloy, which retains the superior properties of titanium while further enhancing biocompatibility, marking a revolutionary breakthrough in dental implant technology.
Today, dentists can choose from a variety of implant materials, including titanium-zirconium alloys, based on the specific needs and oral conditions of their patients. These materials not only offer excellent compatibility with human tissues but also exhibit remarkable resistance to fracture and corrosion.
Titan
Titanium, as the preferred material for dental implants, has been successfully used in clinical applications for decades and is widely recognized for its excellent performance. Titanium not only effectively promotes the process of osseointegration, where the implant bonds closely with the surrounding bone to provide a stable foundation for tooth replacement, but also offers the advantage of relatively low cost. Within the first week after implant surgery, the bone begins to fuse with the titanium implant, and this osseointegration process continues to ensure the long-term stability of the implant. According to statistics, dental implants made from titanium and titanium alloys have a success rate of up to 95%. With proper maintenance, the implant can even last a lifetime. Titanium implants typically consist of two parts: the implant screw (which mimics the natural tooth root) and the abutment (which connects the screw to the crown). This cleverly designed two-piece system allows the implant to penetrate deep into the bone, ensuring a more secure fixation.
Zirkoniumdioxid
Zirconia dental implants are a new option in modern dentistry, offering a highly natural appearance that closely resembles the color of real teeth, making them aesthetically pleasing. The unique white color of zirconia blends perfectly with the patient’s oral environment, achieving a more natural aesthetic result. Compared to titanium implants, zirconia implants feature a simplified one-piece design, streamlining the surgical process and making the treatment more efficient and convenient. Additionally, zirconia exhibits lower sensitivity to allergic reactions and may reduce the risk of inflammation or infection, making it a safer option for certain patient groups, such as those allergic to titanium.
However, it is important to note that despite the many advantages of zirconia implants, they are relatively more brittle and require a higher level of surgical precision. As a newer technology, zirconia implants also lack extensive long-term data on their safety and efficacy, and further clinical studies and observations are needed to validate their long-term outcomes. Nonetheless, for patients seeking a balance of aesthetics and functionality, zirconia implants are undoubtedly a promising and worthy treatment option.
titanium-zirconium alloy
DentalMaster’s titanium-zirconium alloy implant is a dental implant made using advanced material technology. This alloy combines titanium (Ti) and zirconium (Zr) in a specific ratio, commonly Ti15Zr, leveraging titanium’s excellent biocompatibility and zirconium’s high strength. The titanium-zirconium alloy implant not only boasts exceptional mechanical strength, capable of withstanding significant biting forces, but also reduces the risk of post-implant rejection and infection due to its outstanding biocompatibility.
DentalMaster’s titanium-zirconium alloy implants undergo rigorous testing and validation, including assessments of elemental content, metallographic and microstructure analysis, surface properties, mechanical performance, and sterility. These evaluations meet the requirements of relevant medical device registration and internal testing regulations, ensuring both safety and effectiveness, providing patients with reliable quality assurance.
Are There Alternative Materials for Dental Implants?
In the field of dental implants, while titanium and zirconia dominate due to their exceptional biocompatibility and durability, researchers continue to explore other potential materials as alternative options. Here’s a refined and comprehensive overview of these non-traditional materials:
- Ceramic Materials: Advanced ceramics, such as silicon carbide composites, have emerged as attractive options in dental implants due to their excellent durability and chemical stability. These materials are not only aesthetically pleasing, blending naturally with the oral environment, but also offer remarkable biocompatibility. However, their inherent brittleness limits their use in high-stress environments, necessitating more precise surgical techniques and postoperative care to ensure long-term stability.
- Polymer Materials: Polymers, a class of emerging biomaterials, are gaining attention for their biodegradability and customizable properties. In dental implants, polymers can be designed to closely mimic the appearance and texture of natural teeth, offering patients a more personalized aesthetic experience. However, compared to traditional metals, polymers still face challenges in terms of durability, requiring further technological advancements to improve their longevity.
- Alternative Metals: In addition to titanium and zirconia, metals like stainless steel, gold, and cobalt-chromium alloys have been used in dental implants. These metals offer excellent durability and corrosion resistance, providing stable support for patients. However, their biocompatibility may not match that of titanium and zirconia, and in some cases, they may result in higher failure rates. Therefore, when considering these alternative metals, it’s essential to take into account the specific needs and oral health conditions of the patient.
As we discussed earlier, the introduction of titanium-zirconium alloy implants also signifies the ongoing evolution of dental materials. With continuous advancements in materials science and medical technology, we can anticipate more innovative materials emerging in the future, opening up new possibilities and breakthroughs in the field of dental implants.
Dental implant process
The dental implant process is relatively complex yet precise, and the type of implant and the condition of the jawbone will determine how the surgery is carried out. Generally, the process can be divided into the following key steps:
- Pre-Operative Preparation and Evaluation
Oral Examination: A comprehensive oral examination is conducted, including X-rays and CT scans, to assess the patient’s oral health, bone volume, and periodontal condition.
Implant Plan Development: Based on the examination results, the doctor discusses and creates a personalized treatment plan with the patient, deciding on the type, number, and location of the implants.
Pre-Surgical Preparation: Necessary tests such as blood work and ECGs ensure that the patient is fit for surgery. - Implant Surgery
Local Anesthesia: The patient is given local anesthesia to minimize pain and discomfort during the procedure.
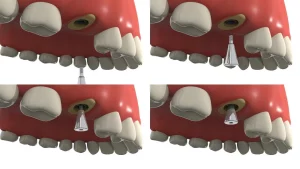
Gum Incision: An incision is made in the gum to expose the alveolar bone where the implant will be placed.
Preparing the Implant Site: Surgical tools are used to create a cavity in the bone to accommodate the implant.
Inserting the Implant: The implant (typically made from titanium) is inserted into the prepared cavity and secured firmly.
Gum Suturing: The gum is sutured to promote healing. - Healing Phase
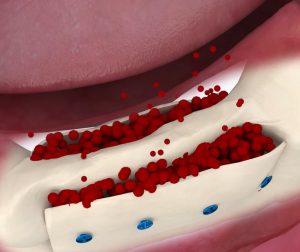
Bone Integration: After the implant is placed, a healing period of 3-6 months is needed for the implant to integrate with the surrounding bone tissue.
Installing a Healing Abutment: Once bone integration is complete, a healing abutment is placed to shape the surrounding soft tissue in preparation for the crown. - Crown Placement
Impression Taking: After the soft tissue has healed, the doctor removes the healing abutment and takes an impression for creating the dental crown.
Crown Placement: The custom-made crown is installed onto the implant, with adjustments made to ensure it matches the appearance and bite alignment of the surrounding teeth. - Post-Operative Care and Follow-Up
Post-Surgical Care: Patients must follow the doctor’s instructions during the recovery period, including medication, oral hygiene, and dietary recommendations.
Regular Check-ups: Routine follow-ups and oral hygiene maintenance are essential for the long-term success of the implant. The doctor will develop a follow-up schedule based on the patient’s needs to ensure the implant remains stable and functional.
In summary, the dental implant process requires close cooperation between the patient and the doctor. Following the treatment plan and adhering to post-operative care instructions is crucial for achieving the best results.
Who are not suitable for dental implants?
- Individuals with severe gum disease: Conditions like gingivitis or periodontitis can damage the gum tissue and underlying alveolar bone, leading to bone loss. Since dental implants require a solid bone foundation to support the implant, patients with insufficient bone structure may experience implant failure. It is recommended to treat and control gum disease first, and if necessary, undergo bone regeneration or bone grafting to increase bone mass before proceeding with dental implant surgery.
- Patients with insufficient jawbone structure: Some patients may have inadequate jawbone due to congenital conditions or external factors (e.g., bone resorption from long-term tooth loss), which may not be able to support an implant. These patients typically need bone augmentation procedures, such as bone grafting or regeneration, to enhance bone density and height to meet the requirements for dental implants.
- Individuals with uncontrolled systemic diseases: Conditions like uncontrolled diabetes, blood clotting disorders, or severe immune system diseases may impair wound healing, increase infection risks, or lower the success rate of the surgery. Therefore, a comprehensive evaluation of the patient’s overall health is required before proceeding with dental implant surgery to ensure safety and efficacy.
- Individuals with poor oral habits: Long-term smoking, excessive alcohol consumption, and other harmful habits can deteriorate oral health, compromising the stability and success rate of implants. These patients are advised to improve their lifestyle before considering dental implant surgery.
- Patients with overly high psychological expectations: While dental implants can restore the function and appearance of teeth, they cannot perfectly replicate natural teeth. For patients with unrealistically high expectations, doctors may suggest reconsidering the decision to undergo the procedure.
Dental Implant Care
Although dental implants are crafted from high-quality, durable materials, their long-term success heavily depends on meticulous care. To maintain the appearance and function of your implants, daily care is essential. It is recommended to brush at least twice a day with a soft-bristled toothbrush and toothpaste specially designed for implants. Additionally, use dental floss or an interdental brush to thoroughly remove food particles between teeth, ensuring a clean oral environment and healthy gums.
Regular professional check-ups are equally important. It’s advisable to visit your dentist every six months for a comprehensive evaluation of your gum health and implant stability. This allows for early detection and resolution of potential issues. Since gum disease is relatively common in dental implant patients, neglecting daily care can lead to peri-implantitis, which may compromise the success and longevity of your implants.
Moreover, dietary habits should be adjusted by minimizing the consumption of sugary drinks, acidic foods, and heavily pigmented items to prevent tooth erosion or discoloration. Avoid biting hard objects or using your teeth as tools, such as opening bottles or chewing ice, to prevent damage or loosening of the implant.
The Future of Dental Implant Technology
As dental implants become the standard solution for missing teeth, the field of dentistry is undergoing unprecedented technological advancements. Dental professionals and researchers are relentlessly working on developing more advanced and efficient implant materials and techniques, aiming to provide patients with a more comfortable and precise treatment experience.
Looking ahead, the prospects for the dental implant market are extremely promising. It is anticipated that the global market value for dental implants will soon surpass the $13 billion milestone. This growth trend reflects the surge in patient demand and underscores the exceptional effectiveness of implant technology in addressing tooth loss. As new patients continue to enter the market, the focus will increasingly be on personalized treatment plans, taking into account factors such as patient allergies and overall health to deliver more tailored and comprehensive care.
In terms of materials science, future advancements in dental implant technology are expected to bring about innovative breakthroughs. Researchers are actively exploring new implant materials aimed at improving biocompatibility, accelerating bone integration, and reducing postoperative complications. Additionally, stem cell technology, as a cutting-edge science, holds promise for playing a significant role in dental implants, offering new possibilities for tooth regeneration and repair. The emergence of these alternative solutions will greatly diversify treatment options, providing patients with more choices.
Furthermore, with the deepening application of digital technologies, dental implant procedures will become more precise and efficient. Advanced technologies such as 3D scanning and virtual surgical planning will allow for accurate preoperative assessments of the patient’s oral condition and the design of personalized surgical plans. This not only helps reduce surgical risks and improve success rates but also allows patients to better understand the procedure in advance, enhancing their confidence and satisfaction with the treatment.