Dental surgery brings hope to countless individuals seeking bright smiles. When you lose one or more teeth due to infection, trauma, or decay, your dentist may recommend dental implants as an effective solution. While the process of implanting the implant and abutment may seem mysterious and challenging to some, it’s essential to understand its components.
Dental implant technology primarily consists of three core components:
- Implant: Often referred to as the “post” or “artificial root,” this is the foundational structure anchored into the jawbone.
- Abutment: Acting as a connecting bridge, the abutment links the implant to the restoration above.
- Restoration: This includes artificial crowns, bridges, or dentures that restore the natural appearance and function of teeth.
In this article, we will focus on and delve into the crucial connecting part of this technology—the abutment.

What is an Abutment?
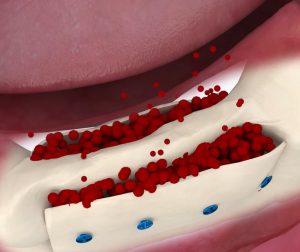
The abutment serves as the bridge between the dental implant and the artificial teeth above, such as crowns, bridges, or dentures, ensuring a secure connection for the restoration. As a crucial component of this intricate system, it is typically crafted from high-quality materials like titanium, zirconia, gold, or stainless steel to ensure durability and biocompatibility.
When considering dental implant surgery, your dentist will recommend the most suitable abutment material, surgical plan, and timing for installation based on your specific situation, including the type of restoration needed, oral health status, and personal preferences. Sometimes, the abutment can be implanted alongside the implant during the initial surgery; in other cases, it may require a secondary surgery after the implant has successfully fused with the jawbone.
Abutments come in various designs to meet different restoration needs. For example, when restoring a single crown, the abutment is often designed like a short screw, tightly connecting the implant to the crown above. Additionally, the connection methods between the abutment and implant vary, utilizing internal hexagonal channels (internal connection) or external hexagonal structures (external connection) at the implant’s top. These designs aim to provide a stable and precise connection, ensuring the long-term stability and functionality of the restoration.
Healing Abutments, Temporary Abutments, and Final Abutments
Abutments play a crucial role in dental implant surgery and can be classified into healing abutments, temporary abutments, and final abutments based on their usage stage and purpose. Here’s a detailed introduction to these three types of abutments:
Healing Abutments (A Type of Temporary Abutment)
Definition and Function: Healing abutments are typically used in the early stages after implant placement. Their main function is to seal the cavity of the implant, preventing bacteria, food debris, and other contaminants from entering and causing infection. They also guide the gum tissue to form appropriately, facilitating the subsequent placement of the crown.
Materials and Shape: Healing abutments can be made from materials such as titanium or PEEK (polyether ether ketone). They may come in various shapes, including conical, cylindrical, or composite, to fit different implant platforms and oral environments.
Timing of Use: After the implant has been placed in the bone and has integrated successfully, the doctor will install the healing abutment during a secondary surgery, allowing the gum tissue to gradually form around it.
Temporäre Abutments
Definition and Function: Temporary abutments are used at certain stages after implant placement to temporarily connect the implant to the restoration (such as a temporary crown), providing initial dental function and aesthetic appeal. While temporary abutments can be similar in function and form to healing abutments, they focus more on immediate dental restoration.
Timing of Use: Temporary abutments may be installed after healing abutments or when the implant and gum tissue have reached a certain level of healing to support the stability of the temporary restoration.
Final Abutments
Definition and Function: Final abutments serve as the last abutment in dental implant surgery, being fixed long-term to the implant to support and stabilize the crown. The design and material selection for final abutments are more refined to ensure a perfect fit and long-term stability with the implant and restoration.
Materials and Shape: Final abutments are typically made from high-quality materials (such as titanium or zirconia), with shapes and sizes precisely designed and manufactured to meet the needs of various restorations.
Timing of Use: Once the implant has fully healed and the gum tissue is stable, the doctor will install the final abutment during a subsequent surgery, after which the appropriate dental crown can be placed.
In summary, healing abutments, temporary abutments, and final abutments each play distinct roles in dental implant surgery, collectively forming a stable foundation for the implant system. When selecting and using abutments, doctors will make personalized recommendations and arrangements based on the patient’s specific needs and circumstances.
Abutment Materials
Abutments can be made from a variety of materials, all of which typically possess good biocompatibility and mechanical properties to ensure the stability and durability of dental implants. Here are some common materials used for abutments:
- Titanium Alloys: Titanium alloys are one of the most commonly used biomaterials for implants due to their excellent biocompatibility, corrosion resistance, and tissue inertness. Using titanium alloys for abutments helps reduce the risk of rejection and promotes the health of both soft and hard tissues.
- Pure Titanium: Pure titanium is another frequently used implant material, known for its superior biocompatibility and mechanical properties. Abutments made from pure titanium effectively avoid metal allergy reactions and provide stable support.
- Zirconia: Zirconia offers high strength and good biocompatibility, making it suitable for creating abutments. Zirconia abutments can enhance comfort and reduce the risk of infection.
- Cobalt-Chromium Alloys: Cobalt-chromium alloys have good mechanical properties and biocompatibility, making them a common choice for abutment materials. Using cobalt-chromium alloys provides stable support without causing allergic reactions.
- Zirconium Oxide: Zirconium oxide is a high-strength ceramic material known for its aesthetic appeal and biocompatibility, making it suitable for abutments. Zirconium oxide abutments have high wear resistance and compressive strength, making them less prone to wear or deformation over time.
Additionally, other materials such as ceramics and porcelain may also be used to create abutments. The choice of material depends on the specific circumstances of the patient and the surgical plan. When selecting abutment materials, the dentist will consider the patient’s oral health status, allergy history, budget, and personal preferences to ensure the most suitable material is chosen.
How Abutments Are Placed
The placement of abutments is a crucial step in dental implant surgery, and the timing and method of placement can vary based on the patient’s specific situation and surgical plan. Here’s a detailed explanation of how abutments are placed:
Timing of Placement
- Simultaneous Placement during Initial Surgery: In some cases, the abutment can be placed at the same time as the implant. This is typically applicable to patients expected to heal quickly and with good bone quality.
- Subsequent Surgery Placement: More commonly, the abutment is placed during a secondary surgery several months after the implant has been placed (usually 3 to 6 months), once the implant has successfully integrated with the bone.
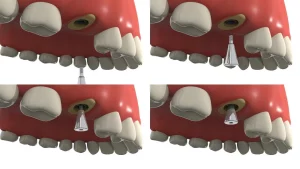
Placement Steps
- Expose the Implant: The doctor will make a small incision in the surgical area to expose the top of the original implant. This usually involves removing some gum tissue and carefully separating the soft tissue to reveal the bone surface and implant.
- Prepare the Abutment: The appropriate abutment is selected based on the type and specifications of the implant. Abutments are typically made from titanium or other biocompatible materials, and their shape and size should match the implant.
- Place the Abutment: The doctor will position the abutment on top of the implant and secure it using appropriate tools (such as screws or adhesives). During this process, the doctor will ensure that the connection between the abutment and the implant is tight and stable.
- Suture and Care: After placing the abutment, the doctor will suture the surgical area to promote healing. Patients must follow postoperative care instructions, including taking antibiotics and maintaining oral hygiene.
- Healing and Follow-Up: After the abutment is placed, the patient needs to wait for a period (typically 4 to 6 weeks) for the gum tissue to heal. During this time, the doctor will schedule follow-up visits to monitor the healing process.
Once the gum has healed well and the connection between the implant and abutment is stable, the patient can proceed to the next phase of restoration, such as placing the crown.
Abutment Post-Operative Care
Post-operative care for abutments requires patients to pay attention to multiple aspects, including immediate post-operative care, oral hygiene maintenance, regular check-ups and follow-ups, and lifestyle adjustments. Proper care is essential to ensure the success and long-term stability of dental implants.
1. Immediate Post-Operative Care
- Avoid Irritating the Wound: After surgery, patients should avoid irritating the surgical area by refraining from vigorous rinsing and sucking on the wound to reduce the risk of bleeding and infection.
- Diet Adjustments: Patients should opt for lukewarm, soft foods and avoid overly hot, hard, or spicy foods to prevent injury to the wound or hinder healing.
- Medication Use: According to the dentist’s advice, patients may need to take antibiotics or anti-inflammatory medication to prevent infection. It’s crucial to take medications on time and in the correct dosage, while also monitoring for any potential side effects.
2. Oral Hygiene Maintenance
- Regular Rinsing: Patients should rinse their mouths after waking, before sleeping, and after meals to minimize bacterial residue and help avoid infection. A saline solution or mouthwash recommended by the dentist can be used for rinsing.
- Careful Brushing: While brushing, patients should control the pressure and duration to avoid excessive force or prolonged brushing, which may damage the implant. Avoid brushing the surgical area for one week post-surgery to prevent irritating the wound.
- Use of Dental Floss: Flossing between the implant and adjacent teeth helps remove food debris and plaque that brushing alone may miss.
3. Regular Check-Ups and Follow-Ups
- Scheduled Check-Ups: Patients should attend regular follow-up appointments as advised by their dentist to monitor the condition of the implant and address any issues promptly.
- Follow-Up Care: If any discomfort or abnormal symptoms such as pain, swelling, or bleeding occur during the use of the implant, patients should contact their dentist for follow-up care.
4. Lifestyle Adjustments
- Avoid Strenuous Exercise: For some time after surgery, patients should avoid vigorous physical activities to prevent increased blood flow that could affect wound healing.
- Quit Smoking and Limit Alcohol: Smoking and drinking can negatively impact oral health, so patients should strive to quit smoking and limit alcohol consumption.
- Maintain a Good Sleep Routine: Adequate sleep and a regular routine contribute to recovery and healing.