In modern dentistry, Guided Bone Regeneration (GBR) has increasingly become a key technique for restoring missing teeth, improving oral function, and enhancing aesthetic outcomes. When the alveolar bone undergoes resorption due to disease, trauma, or prolonged tooth loss, traditional implant restoration often faces the challenge of insufficient bone volume. GBR technology utilizes a combination of biological material barriers and growth factors to precisely guide bone regeneration in targeted areas, providing a stable foundation for implants. This innovative technique, which integrates biological principles with material science, not only overcomes the limitations of traditional bone augmentation procedures but also redefines dental treatment standards with its high predictability and minimally invasive approach. In this article, we will explore the core concepts, surgical procedures, and technical aspects of GBR dentistry, unveiling the science behind this cutting-edge treatment.
What does GBR stand for in dentistry?
Guided Bone Regeneration (GBR) is a key technique in dentistry for repairing alveolar bone defects. It utilizes biocompatible membranes, such as collagen membranes and titanium membranes, to create a physical barrier that prevents soft tissue infiltration. Combined with growth factors like Bone Morphogenetic Protein (BMP) and Platelet-Rich Plasma (PRP), GBR precisely guides bone regeneration in specific areas. This technique not only facilitates vertical and horizontal bone augmentation to address bone deficiency caused by disease, trauma, or prolonged tooth loss but also provides a stable foundation for implant osseointegration, reducing the risk of implant failure.
GBR is widely used in pre-implant bone augmentation, immediate implant restoration, and aesthetic zone reconstruction, particularly for complex bone defects such as vertical bone loss. Compared to traditional bone augmentation techniques, GBR offers minimally invasive procedures, controlled regeneration, and shorter healing times, making it an ideal choice for patients seeking both functional and aesthetic restoration. It is considered the “gold standard” for managing complex bone deficiencies.
GBR Dental Meaning: What It Is and Why It’s Needed
Guided Bone Regeneration (GBR) is a revolutionary technique in the field of dentistry. It aims to precisely guide bone regeneration in specific areas using a combination of biomaterials and growth factors to repair alveolar bone defects caused by disease, trauma, or prolonged tooth loss. The core value of GBR lies in providing sufficient bone support for implant placement or tooth restoration. Particularly for patients with insufficient bone volume or poor bone quality, GBR plays a crucial role in achieving both functional and aesthetic restoration.
Explanation of GBR in dental care
GBR promotes bone regeneration through the following mechanisms:
- Barrier Function: A biocompatible membrane (e.g., collagen membrane, titanium membrane) covers the bone defect area, physically isolating soft tissues (such as gingiva) to prevent their invasion into the bone regeneration space, ensuring bone cells grow in the designated area.
- Growth Factor Activation: The use of bioactive substances such as Bone Morphogenetic Protein (BMP) and Platelet-Rich Plasma (PRP) accelerates the migration, proliferation, and differentiation of bone cells, promoting new bone formation.
- Application Scenarios:
- Pre-implant Bone Augmentation: Reconstructs bone structure for patients with alveolar bone resorption to ensure implant stability.
- Immediate Implant Restoration: Fills extraction socket defects immediately after tooth extraction, reducing treatment time.
- Aesthetic Zone Restoration: Enhances gum contour and prevents soft tissue collapse in the anterior region for improved aesthetic outcomes.
Common reasons for bone loss in the jaw
Jawbone loss results from multiple factors, including:
- Periodontal Disease: Bacterial infections cause inflammation and alveolar bone resorption, making it the most common cause of bone loss.
- Long-term Tooth Loss: Without chewing stimulation, alveolar bone gradually resorbs.
- Trauma or Surgery: Jaw fractures, extractions, and other injuries can damage bone structures, leading to bone loss.
- Systemic Diseases: Conditions such as osteoporosis and diabetes affect bone metabolism, accelerating bone loss.
- Improper Restorations: Poorly designed dentures or implants may exert excessive pressure on bone tissue, causing localized bone resorption.
How GBR helps in dental implant success
GBR provides essential support for successful dental implantation:
1. Bone Volume Enhancement:
- Vertical Bone Augmentation: Addresses insufficient alveolar bone height to ensure proper implant depth.
- Horizontale Knochenaugmentation: Expands alveolar bone width to accommodate implants of different diameters.
2. Improved Implant Stability:
- Newly regenerated bone integrates with the implant, reducing the risk of implant failure.
- Prevents implant loosening or loss due to insufficient bone support.
3. Shortened Treatment Duration:
- Immediate implant placement combined with GBR allows simultaneous extraction, bone augmentation, and implant placement, reducing patient visits.
4. Optimized Aesthetic Outcomes:
In the anterior region, GBR enhances gum contour and prevents post-implant “black triangle” gaps or gum recession.
GBR technology scientifically guides bone regeneration, addressing the challenges of alveolar bone deficiency and significantly improving the success rate and aesthetics of implant restoration. Its precision, efficiency, and predictability make it an indispensable core technology in modern dentistry, offering an optimal functional and aesthetic solution for patients with missing teeth.
GBR Dental Procedure: Step-by-Step Guide
GBR surgery utilizes the synergistic effects of biomaterials and growth factors to precisely guide bone regeneration, creating optimal conditions for implant placement. Below is a detailed breakdown of the procedure:
Step 1: Patient Evaluation and Treatment Planning
Clinical Examination & Imaging Analysis
- Oral Examination: Assess the condition of soft and hard tissues in the edentulous area, the health of adjacent teeth, and occlusal relationships.
- CBCT Scan: Use 3D imaging to determine the extent of alveolar bone defects (height, width, density) and identify nearby anatomical structures (such as the maxillary sinus or inferior alveolar nerve).
Risk Assessment
- Screen for systemic diseases (e.g., diabetes, osteoporosis) that may affect bone healing.
- Evaluate local risk factors such as smoking history and oral hygiene habits.
Customized Treatment Plan
- Select GBR techniques based on defect type (horizontal/vertical deficiency), such as the tenting technique or onlay grafting.
- Determine whether additional procedures (e.g., sinus lift) are necessary.
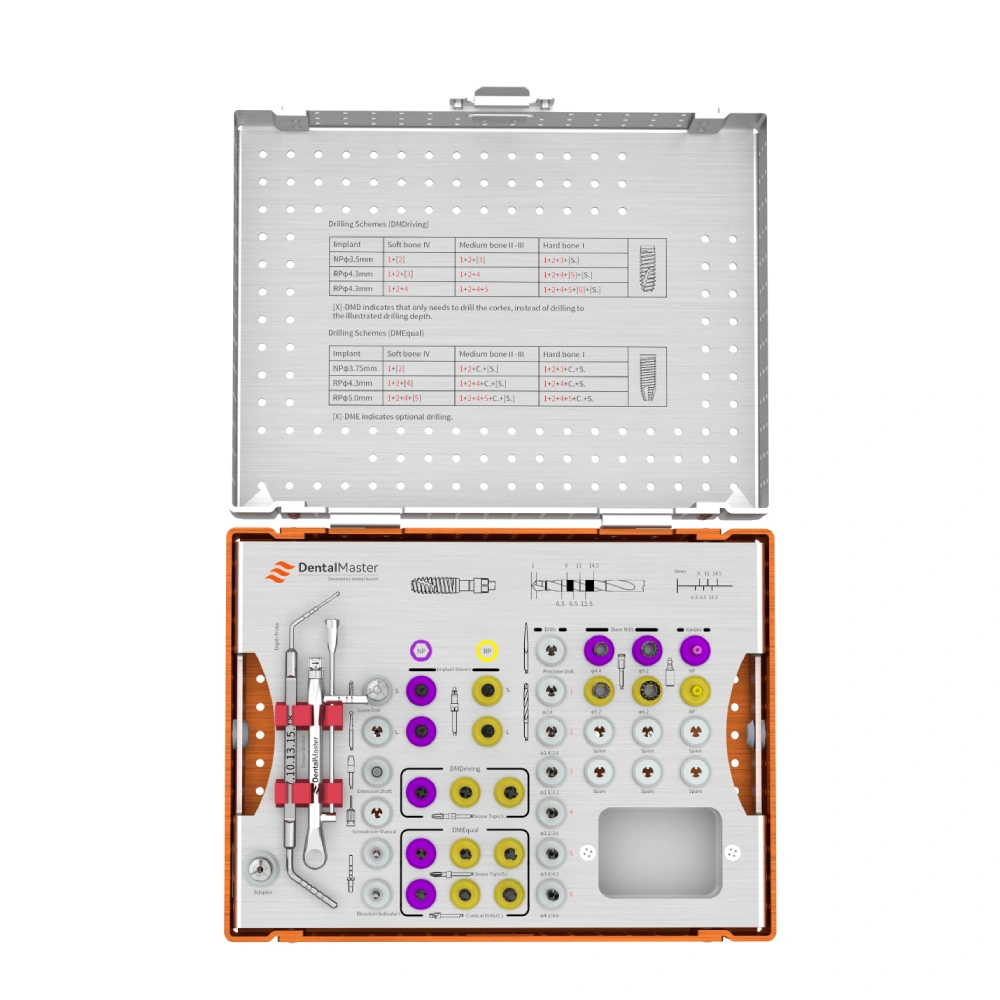
Step 2: Selection of Bone Graft Material and Membrane
Bone Graft Materials
- Autograft: Harvested from the patient’s mandible, iliac crest, etc.; offers high osteogenic potential but involves donor site trauma.
- Allograft: Sterilized human donor bone; avoids donor site morbidity but carries a risk of immune rejection.
- Synthetic Bone Substitutes: Materials like β-tricalcium phosphate (β-TCP) or hydroxyapatite (HA); resorbable and easy to handle.
- Composite Grafts: A combination of autograft and synthetic materials to balance osteogenic potential and convenience.
Barrieremembranen
- Resorbable Membranes (e.g., Collagen Membranes): No need for removal but have lower mechanical strength.
- Non-resorbable Membranes (e.g., Titanium Mesh): Provide excellent stability but require a second surgery for removal.
Growth Factors
- PRP (Platelet-Rich Plasma): Extracted from the patient’s blood via centrifugation to accelerate cell proliferation.
- BMP (Bone Morphogenetic Protein): Stimulates mesenchymal stem cells to differentiate into osteoblasts.
Step 3: Surgical Placement of Graft and Barrier Membrane
Local Anesthesia & Incision Design
- Make an incision in the buccal/palatal mucosa of the edentulous area to expose the bone defect.
Bone Defect Preparation
- Remove infected or necrotic bone tissue and contour the bone edges to improve membrane adaptation.
Graft Placement
- Pack the bone graft material tightly into the defect, ensuring no gaps remain.
Barrier Membrane Coverage
- Extend the membrane edges 2-3 mm beyond the defect to prevent soft tissue invasion.
- Inject PRP or BMP beneath the membrane to enhance bone formation.
Verschluss der Wunde
- Suture the mucosa without tension to prevent membrane exposure and infection.
Step 4: Healing and Bone Regeneration Process
Early Healing (1-2 Weeks)
- The membrane isolates soft tissue, creating a protected space for bone regeneration.
- A blood clot forms around the graft, initiating the inflammatory response.
Bone Formation Phase (2-12 Weeks)
- Osteoblasts migrate to the graft surface and begin new bone formation.
- Autografts typically form woven bone within 4-6 weeks, while synthetic grafts require 6-12 weeks.
Bone Maturation Phase (3-6 Months)
- Woven bone gradually remodels into lamellar bone, with density approaching that of natural bone.
- CBCT scans monitor bone regeneration progress.
Step 5: Final Implant Placement
Timing of Implant Placement
- Early Implantation: 4-6 weeks after GBR (if sufficient primary stability can be achieved).
- Delayed Implantation: 3-6 months after GBR (for full bone maturation).
Implantat-Chirurgie
- Reopen the regenerated bone site, drill according to the planned implant position, and place the implant.
- Torque test ensures primary stability (ISQ ≥ 65).
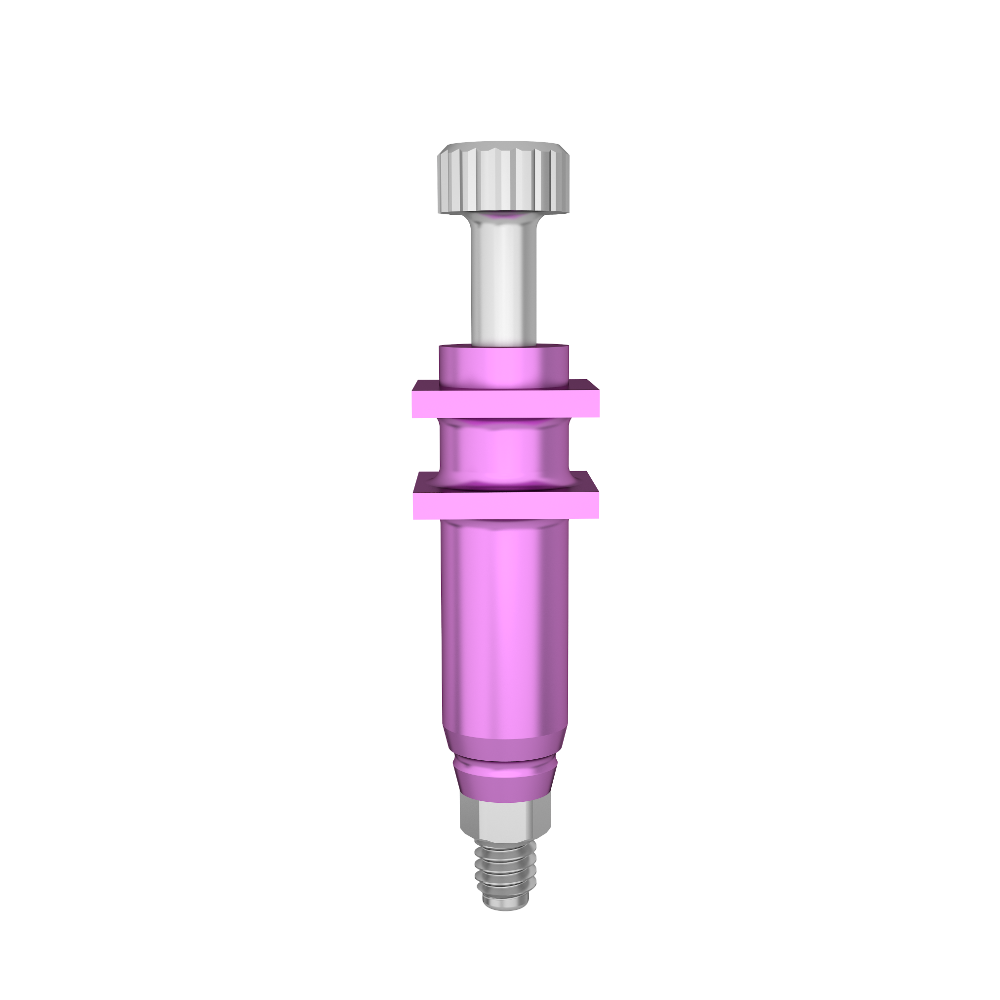
Healing Abutment Placement
- Non-submerged Approach: Immediate healing abutment placement.
- Submerged Approach: Requires a second-stage surgery to expose the implant.
Final Prosthetic Restoration
- After 3-6 months of osseointegration, impressions are taken to fabricate crowns or bridges.
Dental GBR Technology: Methods and Materials
Autografts, Allografts, Xenografts, and Synthetic Bone Graft Materials
In Guided Bone Regeneration (GBR), the choice of bone graft material directly impacts regeneration outcomes and healing speed:
Autotransplantate
- Source: Patient’s own bone tissue (e.g., mandibular bone, iliac crest).
- Vorteile: Best biocompatibility, contains active osteogenic cells and growth factors, promotes fast bone formation.
- Beschränkungen: Requires an additional surgical procedure for bone harvesting, increasing donor site trauma and risk of complications.
Allografts
- Source: Donor bone from the same species (processed through sterilization and decellularization).
- Vorteile: Avoids donor site morbidity and provides structural support for bone regeneration.
- Beschränkungen: Potential risk of immune rejection or disease transmission, lower osteogenic activity compared to autografts.
Xenotransplantate
- Source: Animal bone (e.g., bovine or porcine bone), processed for protein removal and sterilization.
- Vorteile: Readily available and cost-effective.
- Beschränkungen: Lower biocompatibility, unpredictable resorption rate, potential inflammatory response.
Synthetic Bone Graft Materials
- Types: β-Tricalcium Phosphate (β-TCP), Hydroxyapatite (HA), Bioactive glass.
- Vorteile: Customizable shapes, no immunogenicity, controlled resorption rate to match bone regeneration.
- Beschränkungen: Lack of cellular activity, requiring host osteogenesis for bone formation.
Selection Principles: A combination of autografts and synthetic materials is often used to balance regenerative potential and practicality, considering defect size, patient health, and cost factors.
Resorbable vs. Non-Resorbable Membranes
Barrier membranes are a key component of GBR, and their type affects surgical ease and postoperative management:
Resorbierbare Membranen
- Materialien: Collagen (natural) or polylactic acid (PLA, synthetic).
- Vorteile: No need for a second surgery for removal, reducing patient discomfort; supports early soft tissue healing.
- Beschränkungen: Lower mechanical strength, risk of early degradation, potential membrane exposure.
Non-Resorbable Membranes
- Materialien: Titanium mesh or expanded polytetrafluoroethylene (e-PTFE).
- Vorteile: High strength and stability, maintains regeneration space for a longer duration.
- Beschränkungen: Requires a second surgery for removal, potential infection risk or bone resorption around the membrane.
Application Strategies:
- Non-resorbable membranes are preferred for vertical bone augmentation oder high-risk areas requiring extended stability.
- Resorbable membranes are favored for horizontal augmentation oder aesthetic zone reconstructions to simplify treatment.
Advancements in GBR Techniques and Processes
Recent developments in GBR have improved predictability and efficiency through material innovation and digital tools:
Biomaterial Enhancements
- Nanostructured materials: Nanohydroxyapatite coatings improve cell adhesion and osteogenic differentiation.
- Drug-loaded membranes: Barrier membranes infused with antibiotics or growth factors (e.g., BMP-2) for localized, controlled release.
Digital-Assisted Design
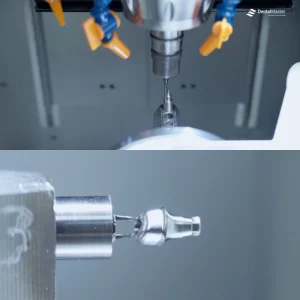
- 3D Printing Technology: Customizes bone grafts and membranes to precisely match defect morphology.
- Dynamic Navigation Surgery: Combines CBCT and optical scanning for real-time guidance in bone graft placement, minimizing trauma.
Minimally Invasive and Accelerated Healing Approaches
- Minimally invasive flap techniques: Reduce incision size, lowering postoperative swelling and pain.
- Concentrated growth factor technology: Uses centrifugation to extract high-concentration PRP, accelerating bone regeneration.
Advanced Regeneration Mechanisms
- Stem Cell Therapy: Utilizing adipose-derived stem cells (ADSCs) or dental pulp stem cells to enhance osteogenesis.
- Immunomodulation: Modifying biomaterials or incorporating anti-inflammatory agents to create an optimized local environment for regeneration.
The evolution of GBR materials and techniques has significantly improved bone regeneration predictability and clinical efficiency. Innovations in biomaterials, barrier membranes, and digital tools have made GBR a precise solution for complex bone defects. With ongoing advancements in biomaterial science and regenerative medicine, GBR is expected to further simplify procedures, reduce healing time, and enhance patient outcomes.
Benefits and Risks of GBR in Dentistry
Advantages of GBR for Dental Implants
Guided Bone Regeneration (GBR) technology utilizes biological barriers and growth factors to provide significant benefits for dental implants:
- Precise Bone Augmentation: Effectively addresses alveolar bone height or width deficiencies caused by periodontal disease, trauma, or long-term tooth loss, expanding implant indications.
- Enhanced Implant Stability: Regenerated bone forms a tight osseointegration with the implant, reducing the risk of post-surgical loosening or failure and extending the lifespan of the prosthetic restoration.
- Aesthetic and Functional Optimization: In aesthetic zone restorations, GBR improves gingival contours and bone profile, preventing post-implant “black triangles” or gum recession, ensuring a natural appearance and proper chewing function.
- Shortened Treatment Duration: When combined with immediate implant placement, GBR allows simultaneous bone augmentation and implant insertion during tooth extraction, reducing patient visits and overall treatment time.
Potential Risks and Complications
Despite its advancements, GBR still presents certain risks:
- Membrane Exposure and Infection: Early exposure of the barrier membrane may lead to bacterial invasion, causing infection or bone regeneration failure, requiring timely intervention (e.g., local antibiotics or membrane removal).
- Donor Site Complications (Autologous Bone Grafting): Bone harvesting may cause pain, bleeding, or nerve damage at the donor site, increasing post-surgical discomfort.
- Abnormal Graft Material Resorption: Some synthetic materials may absorb too quickly or too slowly, potentially affecting bone regeneration quality and necessitating additional surgical adjustments.
- Peri-Implantitis: If bone regeneration is insufficient or postoperative maintenance is inadequate, inflammation around the implant may develop, jeopardizing long-term stability.
Success Rates and Long-Term Outcomes
- Clinical Success Rate: With strict aseptic protocols and personalized treatment planning, the survival rate of implants using GBR reaches 90%-95%, significantly higher than cases without bone augmentation.
- Langfristige Stabilität: Under functional loading, regenerated bone gradually remodels into mature lamellar bone. Five-year follow-up studies indicate that peri-implant bone resorption remains below 1mm per year, ensuring sustained aesthetic outcomes.
- Key Factors for Success: Systemic health conditions (such as diabetes control), postoperative oral hygiene, and smoking habits directly impact long-term success rates, necessitating comprehensive preoperative evaluation and regular follow-ups.
Who Needs GBR Dental Surgery?
Guided Bone Regeneration (GBR) dental surgery is suitable for patients with insufficient jawbone volume or bone defects due to various reasons, including:
Patients with Insufficient Jawbone for Implant Placement
Long-term tooth loss, natural alveolar bone resorption, or failure to restore a tooth after extraction can lead to significant bone loss, making it difficult to support an implant. GBR technology enables vertical and horizontal bone augmentation, precisely reconstructing the bone structure to create optimal conditions for implant placement.
Individuals with Periodontal Disease-Related Bone Loss
Periodontal disease-induced inflammation can destroy the alveolar bone, causing bone resorption and tooth loosening. GBR surgery helps repair bone defects caused by periodontal disease, preventing further bone loss and providing a stable foundation for future implants or restorations.
Patients with Bone Deficiencies Due to Trauma or Congenital Conditions
Injuries such as fractures, surgical trauma, or congenital jawbone underdevelopment (e.g., cleft palate) can result in inadequate bone volume or abnormal bone structure. GBR technology offers customized bone regeneration solutions, restoring the affected area to regain both functional and aesthetic integrity.
Postoperative Care and Recovery for GBR Patients
Healing Timeline and Expected Outcomes
Initial Healing (1-2 Weeks)
- Key Phase: The barrier membrane stabilizes, and a blood clot forms around the grafting material, initiating the inflammatory response.
- Expected Outcome: Soft tissue begins to heal, with mild swelling or bruising gradually subsiding.
Bone Regeneration Phase (2-12 Weeks)
- Key Phase: Osteoblasts migrate to the grafting material’s surface, starting new bone formation.
- Expected Outcome:
- Autogenous bone grafts typically form woven bone within 4-6 weeks.
- Synthetic materials may take 6-12 weeks to integrate.
- CBCT scans reveal increasing bone density over time.
Bone Maturation Phase (3-6 Months)
- Key Phase: Woven bone remodels into lamellar bone, achieving a structure and function similar to natural bone.
- Expected Outcome:
- Stable bone volume, meeting the requirements for implant placement or prosthetic restoration.
- Enhanced implant success rate with stronger osseointegration.
- Improved aesthetics, with natural gum contours in visible areas.
Postoperative Guidelines for GBR Surgery
Wound Care
- Avoid Touching: Do not use your tongue or fingers to touch the surgical site to prevent membrane displacement or infection.
- Cold Compress: Apply an ice pack intermittently during the first 24 hours to reduce swelling.
Diet and Oral Hygiene
- Soft Diet: Stick to soft foods for the first week to prevent wound disruption.
- Gentle Cleaning: Start using chlorhexidine mouthwash after 24 hours, avoiding direct brushing of the surgical site. Resume normal brushing after 7 days.
Activity and Medications
- Vermeiden Sie anstrengende körperliche Betätigung: Refrain from intense physical activity for one week to prevent increased blood pressure and delayed healing.
- Follow Prescription: Take antibiotics and anti-inflammatory medications as directed. Use pain relievers if necessary.
Restricted Activities
- No Smoking or Alcohol: Avoid smoking and drinking for at least 4 weeks to ensure proper bone regeneration.
- Avoid Suction Movements: Do not use a straw to prevent oral pressure changes that may cause bleeding.
Tips for Maintaining Bone Health After GBR
Regelmäßige Kontrolluntersuchungen
- Postoperative Follow-ups: Attend scheduled CBCT scans to monitor bone regeneration progress.
- Implant Maintenance: After implant placement, visit your dentist every 6 months to assess bite alignment and gum health.
Oral Hygiene Management
- Proper Brushing: Use a soft-bristled toothbrush and floss around the implant site to prevent plaque buildup.
- Water Flosser Assistance: Nach 3 weeks, gently clean the surgical area with a water flosser.
Nutrition and Lifestyle Habits
- Ausgewogene Ernährung: Eat calcium-rich foods (e.g., dairy), vitamin D sources (e.g., fish), and protein for optimal bone metabolism.
- Systemic Health Control: Maintain stable blood sugar levels if diabetic to avoid delayed bone healing.
Preventing Complications
- Avoid Trauma: Protect the surgical site from impact or excessive pressure.
- Early Intervention: Contact your dentist immediately if you notice redness, discharge, or fever, as these may indicate infection.
Schlussfolgerung
Guided Bone Regeneration (GBR) technology, as a groundbreaking innovation in modern dentistry, successfully addresses the challenges of alveolar bone resorption through precise regulation of biological barriers and growth factors. It provides a functional and aesthetic restoration solution for patients with tooth loss. The core value of GBR lies not only in precise bone augmentation and enhanced implant stability but also in its minimally invasive, personalized surgical design, which significantly reduces treatment trauma and complication risks, achieving a transformation from “bone defect challenges” to “predictable regeneration.”
Although the implementation of GBR requires strict control over material selection, barrier membrane management, and postoperative care, its high success rate (implant survival rate exceeding 90%) and long-term stability (5-year bone resorption rate less than 1mm per year) have made it the clinical gold standard for complex bone defect repair. By integrating biological principles with material science, GBR not only drives progress in implant dentistry but also opens new avenues for regenerative medicine applications in dentistry.
In the future, with advancements in biomaterial research (such as smart drug-loaded membranes and nanostructured materials) and digital technology (such as dynamic navigation and 3D printing), GBR will further simplify procedures, shorten healing time, and achieve more precise bone regeneration control. The continuous evolution of this technology is expected to enhance the treatment experience and quality of life for patients with tooth loss while redefining the standard paradigm of dental restoration, providing a functional and aesthetic oral health solution for more individuals.