Dental implants are a revolutionary solution for restoring missing teeth, offering both functionality and aesthetic benefits. Whether you have lost teeth due to injury, decay, or disease, dental implants can significantly improve your quality of life by restoring your ability to chew, speak, and smile with confidence. Here’s everything you need to know about dental implants.
Definition and Purpose of Dental Implants
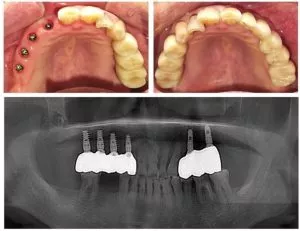
A dental implant is an artificial tooth root that is surgically placed into the jawbone to support a replacement tooth or dental bridge. Unlike traditional dentures or bridges, dental implants provide a permanent solution designed to restore both the function and appearance of natural teeth. They effectively restore chewing and speaking abilities, while significantly boosting the patient’s confidence and quality of life.
When a tooth is lost due to injury, decay, or disease, a dental implant provides a solid foundation to prevent bone loss that typically occurs with missing teeth. The absence of a tooth root can cause the surrounding jawbone to gradually deteriorate. However, dental implants integrate with the bone, stimulating bone growth and maintaining its health and integrity. This not only helps prevent changes in facial structure but also avoids other oral health issues caused by bone loss.
Dental implants consist of three main components: the artificial tooth root (usually made of biocompatible titanium alloy), the abutment that connects the root to the crown, and the customized dental crown that covers the abutment. These components work together, making dental implants function similarly to natural teeth while also appearing almost indistinguishable. With professional design, the color, shape, and size of the implant can be tailored to meet the patient’s specific needs, ensuring perfect integration with the surrounding natural teeth.
Causes of Tooth Loss and Associated Complications
Tooth loss can be caused by various factors, including:
- Injury: Accidents or trauma can cause teeth to loosen or fall out, especially during sports or other high-risk activities.
- Decay: Severe cavities, if left untreated, can destroy the tooth structure, eventually leading to tooth loss.
- Diseases: Gum diseases (such as periodontitis) and other oral infections can damage the tissues supporting the teeth, causing them to loosen and fall out. Additionally, some systemic diseases can affect oral health, increasing the risk of tooth loss.
- Aging: As people age, natural wear and tear on teeth, combined with possible oral health issues, makes older adults more susceptible to tooth loss.
Tooth loss can lead to several complications, including:
- Bone Resorption: After tooth loss, the jawbone may begin to shrink, leading to bone loss. This change not only affects the surrounding teeth but can also cause further tooth loss.
- Speech Problems: Missing teeth can impact pronunciation, causing speech to be unclear or indistinct.
- Chewing Difficulties: Missing teeth limit the ability to chew certain foods, which can affect dietary habits and nutrient intake.
- Aesthetic Issues: Tooth loss can negatively impact facial appearance, making one look older and potentially lowering self-esteem and confidence.
Components of a Dental Implant
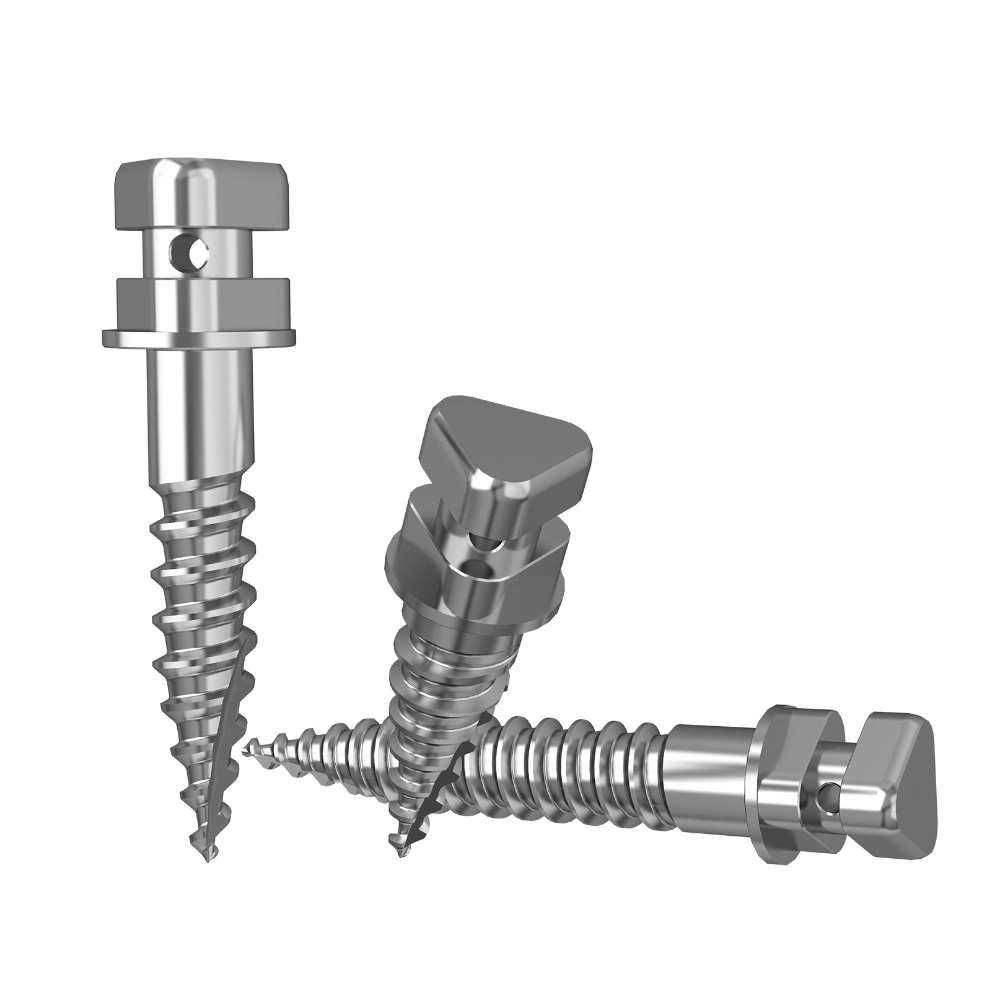
A dental implant consists of three main parts: the implant (root), abutment, and fixation screw. These components work together to provide patients with a stable, durable, and aesthetically pleasing tooth replacement solution. Each part is carefully designed to ensure compatibility with the patient’s oral environment, offering the best functionality and comfort. With professional surgery and follow-up care, dental implants can be an effective solution for restoring oral health and confidence.
- Implant (Root)
- Definition: The implant is the core part of the dental implant system, functioning as the artificial tooth root.
- Material: Implants are typically made of titanium or titanium alloys due to their excellent biocompatibility and strength, allowing them to integrate closely with the jawbone (a process known as osseointegration).
- Function: Surgically implanted into the jawbone, the implant provides a stable foundation for the upper structure (the artificial tooth).
- Abutment
- Definition: The abutment is the component that connects the implant to the artificial tooth. It sits above the implant and protrudes through the gum tissue.
- Material: Abutments can be made of metal (like titanium), ceramic, or composite materials, depending on the patient’s needs and the dentist’s recommendation.
- Function: The abutment not only supports the artificial tooth but also ensures the stability and aesthetics of the final restoration.
- Fixation Screw
- Definition: The fixation screw is a small metal component used to secure the abutment to the implant.
- Material: Fixation screws are typically made of the same material as the implant (e.g., titanium) to ensure stability and durability.
- Function: The fixation screw ensures a firm connection between the abutment and implant, preventing the artificial tooth from shifting or becoming loose.
Pre- and Post-Operative Care for Dental Implants
4.1 Pre-Operative Considerations
Before deciding to undergo dental implant surgery, it is essential to have a thorough and detailed discussion with your dentist. Your overall health, medical history, and smoking habits can all impact the success rate of the surgery. For example, smoking not only delays the healing process but may also increase the risk of implant failure. Therefore, your dentist will evaluate your specific situation to determine if you are a suitable candidate for the procedure.
Here are some key pre-operative steps to follow:
- Oral Health Check-Up: Ensure that there are no infections or other oral health issues. If necessary, treat conditions like gum disease or cavities before proceeding with the implant surgery.
- Maintain Good Oral Hygiene: Keep your mouth clean before the surgery by brushing regularly and using mouthwash to reduce the risk of infection.
- Avoid Smoking and Drinking: It is recommended to minimize smoking and alcohol consumption several days before the surgery, and to avoid them completely on the day of the surgery to promote healing.
- Health Evaluation: Undergo routine blood tests, including blood sugar and blood pressure monitoring. If you have a history of chronic conditions like hypertension or diabetes, be sure to inform your dentist and follow medical advice for medication.
- Prepare for a Proper Diet: On the day of surgery, ensure you have a healthy meal and get plenty of rest to help your body prepare for the procedure.
4.2 Post-Operative Care
After the dental implant surgery, it is critical to follow proper oral hygiene and care to prevent infection and ensure a smooth recovery. Special attention should be given to the gums and implant site. Here are some key post-operative care tips:
- Maintain Oral Cleanliness: Avoid brushing and rinsing your mouth within the first 24 hours to prevent bleeding from the wound. After that, you can rinse with warm salt water to maintain good oral hygiene, but do so gently to avoid irritation.
- Follow-Up Appointments: Visit your dentist for regular check-ups to monitor the stability and healing progress of the implant. If you experience any pain, discomfort, or notice loosening of the implant, contact your dentist immediately.
- Diet Adjustments: Initially, stick to soft foods and avoid hard, hot, or spicy foods to prevent irritation at the implant site. Soft foods like mashed potatoes and yogurt are easy to chew.
- Medication Management: Follow the dentist’s instructions to take antibiotics and pain relievers to prevent infection and alleviate discomfort.
- Avoid Strenuous Activities: During the recovery period, avoid vigorous physical activities or heavy labor that may place pressure on the implant.
In conclusion, understanding and following these pre- and post-operative care instructions will help ensure the success of your dental implant surgery and promote a quick recovery. If you have any concerns or questions about your situation, feel free to consult your dentist.
Benefits and Risks of Dental Implants
5.1 Benefits
- Restoration of Function and Appearance: Dental implants effectively restore chewing and normal speaking abilities, significantly improving overall quality of life. Compared to traditional dentures, implants provide more stable support, allowing patients to enjoy a variety of foods without worrying about the looseness or discomfort of dentures.
- Prevention of Bone Loss: Implants help maintain the structure of the jawbone, preventing bone resorption due to missing teeth. When a tooth is lost, the jawbone that supports the tooth gradually shrinks. The implant, mimicking the natural tooth root, stimulates the bone and helps maintain its density and health.
- Improved Self-Esteem: Having a complete smile can significantly boost confidence and self-esteem. The appearance of dental implants is almost indistinguishable from natural teeth, and when professionally designed, they blend seamlessly into the mouth, allowing patients to feel more confident in social settings.
- Durability: With proper care, dental implants can last for many years, even a lifetime. The materials used, typically titanium alloys with strong biocompatibility, are resistant to cavities and other issues, providing patients with a long-term, reliable solution.
- Maintaining Oral Health: Compared to traditional dentures, dental implants are easier to clean and maintain. Patients can care for them just like natural teeth, regularly brushing and flossing to help prevent oral diseases.
5.2 Risks
- Surgical Complications: Although surgical complications are rare, they can occur. For example, damage to adjacent teeth or tissues during the implantation procedure could cause discomfort or lead to further complications.
- Implant Failure: In some cases, the implant may loosen or the body may reject the implant. Factors affecting the success rate include the patient’s overall health, smoking habits, and oral hygiene.
- Cleaning Issues: Implants require good oral hygiene to avoid plaque buildup, which can lead to gum disease. Failure to properly clean the implant can result in peri-implantitis or other severe issues, affecting the long-term stability of the implant.
- Infection Risk: Infection may occur at the implant site post-surgery. Though rare, if not treated promptly, infections can lead to more serious problems, such as jawbone infections or the need for implant removal.
- Nerve Damage: In some cases, implant surgery may cause damage to surrounding nerves, leading to numbness, tingling, or discomfort. This is usually caused by the implant being placed too close to a nerve, which is why pre-operative imaging is crucial.
Quality Standards and Safety Evaluation of Dental Implants
Dental implants, as medical devices directly applied to the human body, require stringent quality standards and safety evaluations. Below is a detailed analysis of the quality standards and safety assessment for dental implants:
1. International Standards
Dental implants must comply with a series of international standards, which are set by authoritative global organizations to ensure the safety, effectiveness, and biocompatibility of the product. Common international standards include:
- ISO 14607: The standard for dental implants, which covers requirements regarding the design, materials, and performance of implants.
- ASTM Standards: Such as ASTM F2328 (for polymer-based orthopedic implants) and ASTM F2024 (for cranial implants), which specify detailed testing methods and performance requirements for different types of implants.
2. Material Requirements
The material selection for dental implants is crucial, and it must meet the following requirements:
- Biocompatibility: The material must be harmless to the human body, without causing adverse reactions like allergies or rejection. High-quality titanium is commonly used due to its excellent biocompatibility and strength.
- Corrosion Resistance: The material must exhibit good corrosion resistance to prevent deterioration in the oral environment, which could release harmful substances.
- Mechanical Properties: The material must meet specific mechanical performance requirements, such as strength and toughness, to ensure the implant can provide stable support for the upper structure (e.g., crowns or bridges).
3. Biocompatibility Testing
Biocompatibility testing is an essential process to ensure the safety of dental implants. Common biocompatibility tests include:
- Cytotoxicity Testing: Through in vitro cell culture, the material’s impact on cell growth, reproduction, and morphology is observed to evaluate its cytotoxicity.
- Animal Testing: The material is implanted in animals to observe its systemic toxicity and local tissue reactions. These tests simulate the human environment, assessing the material’s biocompatibility and safety.
- Genotoxicity Testing: This test evaluates whether the material induces gene mutations or chromosomal abnormalities, which can indicate potential carcinogenic effects.
4. Safety Evaluation
In addition to the biocompatibility tests mentioned above, the safety evaluation of dental implants also includes the following aspects:
- Preclinical Trials: A series of tests conducted on animal models to assess the material’s toxicity to the targeted tissue area. These trials further validate the biocompatibility and safety of the material.
- Clinical Trials: Trials conducted on humans to evaluate the safety and effectiveness of dental implants. These trials typically involve a large number of patients and require long-term monitoring and data collection.
- Long-Term Follow-Up: Monitoring and tracking patients who have received dental implants to assess long-term safety and outcomes. This helps to identify and resolve potential issues as they arise.
5. Other Considerations
- Quality Control: Strict quality control must be implemented during production to ensure that each implant meets the specified standards and requirements.
- Labeling and Packaging: Implants must be clearly labeled with their model, specifications, production date, etc., and securely packaged to prevent damage during transportation and storage.
- Instructions for Use: Detailed instructions and precautions must be provided to ensure that dentists use the implants correctly and minimize surgical risks.
Conclusion
Dental implants are an ideal solution for individuals with missing teeth, offering both functional and aesthetic benefits. Through dental implants, patients can not only restore their ability to chew and speak normally but also regain their confident smile, significantly improving their quality of life. The design of dental implants closely resembles natural teeth and effectively prevents bone loss, providing a solid foundation for artificial teeth.
Furthermore, the durability of dental implants makes them a long-term solution. With proper care and regular dental check-ups, implants can last many years, improving both oral health and overall quality of life. Compared to traditional dentures, dental implants better preserve the natural state of the mouth without affecting the structure of nearby healthy teeth.
However, before deciding to undergo dental implant surgery, it is crucial to consult with your dentist about all available options and associated risks to ensure that dental implants are the best choice for you. With professional evaluation and personalized treatment plans, you can make an informed decision that will make your smile shine.