Does your clinic completely adhere to the CDC’s Dental Instrument Sterilization Guidelines?
The long-term, efficient use of dental tools depends on proper upkeep and care. In addition to safeguarding your investment in top-notch dental equipment, a safe and effective cleaning procedure also safeguards the health and safety of patients, equipment, and medical personnel.
Cost is not the only consideration here. We are on the front lines of the battle against infections as dental health professionals. One of the most crucial and efficient steps we can take to safeguard our tools, patients, and ourselves is the cleaning and disinfection procedure.
The gold standard for dental clinic operations has long been the CDC’s Guidelines for Infection Control in Dental healthcare settings. Processing instruments is essential to stopping the spread of pathogens. Any microbial residue on dental equipment may easily cause infections since they often come into touch with or enter delicate tissues.
We include some recommended procedures for cleaning dental tools below. You may reduce the chance of infection transmission and prolong the life of your equipment by closely following these guidelines.

1. Personal Protection is Essential
Personal protection equipment (PPE) including gloves, masks, safety goggles, and waterproof gowns are essential for cleaning and arranging dental tools. These things provide a strong barrier that shields you from microbial contamination and keeps any possible infections you could have from contaminating the equipment.
During this technique, protective gloves are very important. When handling dental tools, accidents may happen without warning, but gloves that are resistant to chemicals and punctures provide the protection that is required. These gloves are both reusable and cost-effective since they can be sanitized in high-temperature autoclaves.
certain dentists can gripe that certain gloves are overly heavy and restrict their range of motion. It’s crucial to remember that different gloves have different qualities. Safety and effectiveness go hand in hand because of the abundance of lightweight choices available on the market that provide superior protection without sacrificing comfort or flexibility.
2. Pre-Soaking Instruments
Time restrictions may prevent used equipment from being cleaned right away in busy dental offices. This may create issues because, like dirty dishes left in the sink for too long, biological material, like blood, hardens once it dries. It might be difficult to get rid of the hardened residue when it comes time to clean the equipment.
Experts in infection management advise pre-soaking devices as a preventative strategy to deal with this problem. To keep organic waste wet, contaminated instruments may be sprayed with an appropriate solution. For this, enzyme spray gels are a good choice since they quickly dissolve and get rid of any buildup before the instruments are cleaned, making the procedure run more smoothly.
3. Sterilization Must Follow Cleaning
When dental tools are sterilized in an autoclave, if dirt is still on them, the superheated steam may not reach all of the instrument surfaces, which might compromise the sterilization process. Therefore, it is crucial to completely remove any visible residue from tools prior to sterilization, in accordance with the Centers for Disease Control and Prevention’s (CDC) requirements.
The following cleaning techniques may be used to accomplish this:
- Ultrasonic Cleaning: This technique loosens and gets rid of dirt off instruments by sending sound waves through a solution. In order to ensure efficient cleaning, high-quality ultrasonic cleaning solutions usually include enzymes that degrade impurities and additives to stop mineral deposits, discoloration, and corrosion.
- Automatic Cleaning Equipment: By automating the rinsing and drying processes, these devices greatly save labor costs and time while enhancing cleaning effectiveness and security.
- Manual Cleaning: The CDC does not advise this approach, even though it could be required in some circumstances. In addition to being labor-intensive and time-consuming, manual cleaning raises the possibility of sharps accidents, putting worker safety at risk.
Furthermore, the CDC advises keeping an eye on the cleaning techniques to guarantee their efficacy. Monitoring strips, for instance, may be used to confirm that the cleaning procedure complies with regulations when utilizing ultrasonic cleaners.
4. Ensure Instruments Are Dry
It is crucial to make sure dental equipment are totally dry before putting them in an autoclave. This is due to the fact that an autoclave’s main purpose is to remove moisture produced during the sterilizing procedure, not to get rid of moisture that already exists on the equipment.
In a Dental Economics paper, infection control specialist John A. Molinari pointed out that if tools are put in the autoclave moist, they will stay wet long after the sterilizing procedure is finished. Moisture and germs from the skin may be absorbed by wet packing materials, reducing the effectiveness of sterilization and raising the possibility of recontamination. To guarantee the best outcomes, it is crucial to completely dry equipment before sterilizing them.
5. Proper Packaging of Instruments
In order to avoid re-contamination once the sterilizing procedure is over and the instruments are exposed to the air, dental instruments must be packed in appropriate packaging or bags before being placed in the sterilizer.
When choosing packing materials, it’s critical to make sure they can tolerate high temperatures and pressures and have appropriate sterilizing agent penetration qualities. In order to confirm that the sterilizer has attained the proper temperature, duration, and if steam has effectively permeated the packing, the CDC also advises putting chemical indicators both inside and outside each container.
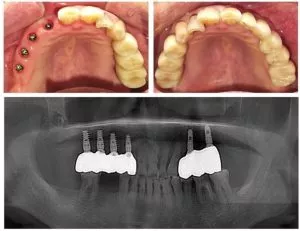
Spore tests, another name for biological indicators, may also be utilized for a more thorough evaluation of sterilization efficacy. The effectiveness of the sterilizer in eliminating very resistant germs, including Geobacillus stearothermophilus, may be determined using this test. A spore test should be conducted at least once per week and while implanted devices are being processed, according to the CDC.
Handle Instrument Loading with Care
Overloading the autoclave is one of the main reasons for sterilization failure, despite the temptation to pack as many devices as possible into each sterilization cycle.
To guarantee that the sterilizing agent can circulate completely and equally to every instrument, DentalMastermed advises positioning packed devices upright on the autoclave racks.
Instrument Trays’ Function
Individual dental tool cleaning and sterilization may be time-consuming and raise the possibility of sharps injury. A single sharps injury typically costs around $3,000, according to the CDC’s Sharps Injury Prevention Manual.
In dental offices, using instrument trays greatly increases productivity and lowers safety hazards. Healthcare professionals may save time while finding and switching equipment during operations by configuring each tray for a particular technique. Additionally, the trays may be placed straight into autoclaves, automated washers, and ultrasonic cleaners. The trays may be carefully kept until they are required after being cleaned and sanitized.
For instance, DentalMaster saves five to ten minutes of preparation time for every surgery by providing trays for all dental surgical kits.
Optimized cleaning and sterilizing procedures protect equipment, patients, and employees, increasing safety and optimizing your clinic’s return on investment.