A crucial technique in contemporary dental implantology is guided bone regeneration (GBR), which allows dentists to replace missing or inadequate bone tissue. This allows dental implants to be placed even in regions with inadequate bone volume. Bone loss in the jaw may significantly restrict the placement of dental implants, regardless of the cause—tooth loss, trauma, or periodontal disease. In order to overcome these obstacles, increase the success rate of dental implant treatments, and improve patient outcomes, GBR has emerged as a game-changing technology.
The idea of guided bone regeneration, its operation, the kinds of materials utilised, the actual technique, and the reasons it is a crucial tool in contemporary dentistry will all be covered in this extensive book.
What is Guided Bone Regeneration?
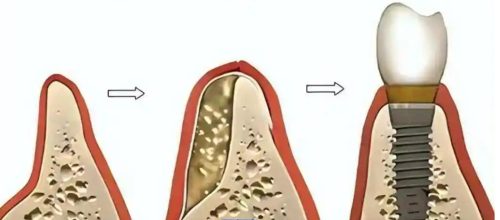
A surgical procedure called guided bone regeneration (GBR) is used to promote the formation of new bone in regions where bone has been lost. In order to successfully insert dental implants, it usually entails the use of barrier membranes to direct bone tissue regeneration in the proper position and form. When there is not enough bone volume to insert implants and when bone loss has occurred in the jaw region where teeth are missing, GBR is often used.
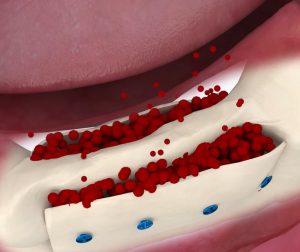
To stop undesirable tissues, including soft gum tissue, from growing into the defect as the bone regenerates, a membrane is applied over the defect region during the surgery. New bone may grow in the vacant region since the membrane serves as a barrier to preserve the regenerative bone tissue. Dental implants may be inserted once the bone has healed and grown adequately.
Why is GBR Necessary?
Bone resorption is the term for the gradual deterioration of the local bone structure after tooth loss. The jawbone, which may shorten considerably after tooth loss, is particularly prone to this. In certain situations, the jaw may not have enough bone mass or quality to hold a dental implant. An implant that will fuse with the bone and act as a natural tooth root is difficult, if not impossible, to put without sufficient bone.
By encouraging the formation of new bone in places that are lacking, GBR helps address this problem. In order to prepare for dental implants, the treatment enables the repair of the bone structure. It is often administered to individuals who have had severe bone loss because of:
Tooth extraction: The surrounding bone may start to deteriorate and shrink once a tooth is gone.
Periodontal disease: Bone loss in the jaw may result from gum disease.
Trauma or injury: Bone loss in the vicinity of a missing tooth may result from facial trauma.
Congenital defects: Genetic factors may cause certain people to have inadequate bone volume.
The Guided Bone Regeneration Procedure
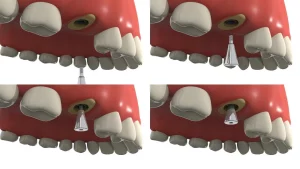
Typically, the GBR process consists of a few essential components. Below is a summary of the usual procedure:
- Consultation and Evaluation
The patient’s dental health, the degree of bone loss, and whether GBR is the best course of action will all be assessed by the dentist or oral surgeon before to the treatment. The bone structure and defect region are evaluated using imaging methods as X-rays or 3D scans (CBCT).
Additionally, the surgeon will look for any underlying issues that can interfere with the healing process, such infection or gum disease. A treatment plan will be created to meet the patient’s unique requirements when the evaluation is finished.
- Incision and Anaesthesia
In order to numb the jaw region where the regeneration is to occur, the patient will usually receive local anaesthesia during the treatment. Depending on the patient’s comfort level or the intricacy of the case, sedation or general anaesthesia may be employed in some situations.
After numbing the region, the oral surgeon will reach the underlying bone by making a little incision in the gum tissue. In order to minimise obvious scarring, the incision is usually done along the gum line.
- Membrane Positioning
The usage of a membrane is essential to the GBR process. While the bone heals, the membrane serves as a barrier to keep soft tissues out of the bone defect. The following membrane types are most often used in GBR:
Resorbable membranes are composed of substances that, over time, decompose and get absorbed by the body. Once the healing process is complete, they don’t need to be removed.
Non-Resorbable Membranes: These membranes are composed of synthetic polymers or titanium mesh. Until a second treatment removes them, they stay in place.
After the membrane has been properly positioned over the bone defect, more bone graft materials could sometimes be utilised to aid in the healing process. These graft materials may come from a variety of sources, such as:
Bone from the patient’s own body is used in autografts.
Bone from a donor (typically cadaveric) is used in allografts.
Xenografts: Animal bones, usually from cows.
Alloplasts: Artificial bone replacements.
- Bone grafting, if necessary
The oral surgeon may also utilise bone grafts in conjunction with the membrane to promote bone regeneration in situations when there has been a substantial loss of bone. The new bone cells may grow onto the structure that these transplants assist to establish. - Healing and Suturing
Following the placement of the membrane and bone grafting material, the surgeon will meticulously sew the incision shut. Although the mending process starts right away, the bone may not totally repair for many months. To achieve appropriate healing during this time, the patient must adhere to the surgeon’s post-operative care guidelines. - Implant placement and follow-up
Following the healing phase, which usually lasts four to six months, the surgeon will assess the newly grown bone to see whether it is strong enough to hold a dental implant. The implant may be inserted into the regenerated bone when it has healed and integrated. - Complete Repair
The crown or prosthetic tooth, the last restoration, may be positioned on top of the implant after it has been inserted and assimilated into the bone. After that, the patient may take pleasure in a completely functioning and beautiful dental repair.
Advantages of Bone Regeneration Under Guidance
There are several benefits to the GBR process for both patients and dentists:
- Bone Structure Restoration: GBR makes it possible to replace missing bone, which is necessary for dental implants to be placed successfully.
- Minimally Invasive: Using tiny incisions and often needing only one surgical visit, the technique is minimally invasive.
- Increased Implant Success Rates: GBR raises the likelihood of a successful dental implant operation by growing bone in places that are lacking.
- Results Over Time: The benefits may remain for many years after the implant is placed and the bone has healed, offering a long-lasting and permanent remedy for tooth loss.
Post-Operative Care and Healing
The healing phase after the GBR operation is essential to the treatment’s effectiveness. Patients should adhere to the post-operative care guidelines that their surgeon has given them, which usually consist of:
- Chewing on the treated region and avoiding hard foods.
- maintaining cleanliness to avoid infection.
- taking painkillers as directed as necessary.
- keeping track of recovery by going to follow-up visits.
Conclusion
A crucial technique in contemporary dentistry, guided bone regeneration allows dentists to replace missing bone and prime the jaw for an implant to be placed successfully. Dental implants are now beneficial for individuals with bone shortages, especially in regions where there has been substantial bone loss, thanks to GBR. The process has transformed dental implantology by offering people who have lost teeth a dependable and efficient way to restore both function and appearance.
Discuss the potential of a Guided Bone Regeneration surgery with your dentist or oral surgeon if you’re thinking about getting a dental implant but are worried about bone loss. GBR may assist in restoring your smile and enhancing your general oral health with the appropriate treatment plan.