AIDS, a serious disease caused by the human immunodeficiency virus (HIV), profoundly affects the immune system of patients, making them more susceptible to various infections and illnesses. In medical settings, especially in dental clinics where close contact is frequent, the survival time of HIV on dental instruments becomes a critical factor in preventing cross-contamination.

Survival Time of HIV on Dental Instruments
The survival time of HIV in the external environment is not fixed; it is influenced by several factors, including temperature, humidity, and the material of the dental instruments. On dental instruments, the survival time of HIV is generally limited, but specific conditions should be examined:
- Dry Environments: In dry conditions, the survival capability of HIV is severely restricted. Studies show that HIV typically survives on the dry surfaces of dental instruments for no more than 24 hours, and often for an even shorter duration. This is because HIV requires a moist environment to maintain its biological activity.
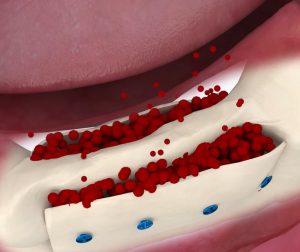
- Moist Environments: In contrast, the survival time of HIV may significantly extend in moist conditions. When there are residues of saliva, blood, or other body fluids on dental instruments, the virus may survive for several days, increasing the risk of transmission through dental tools.
- Material Differences: The materials used for dental instruments also impact the survival time of HIV. Common materials such as metal, plastic, and glass interact differently with HIV. Generally, metal surfaces are less conducive to HIV survival, while plastic surfaces may allow for longer survival times.

Preventive Measures in Dental Clinics
Given the potential survival risk of HIV on dental instruments, dental clinics must implement a series of stringent preventive measures to ensure the safety of patients and healthcare personnel:
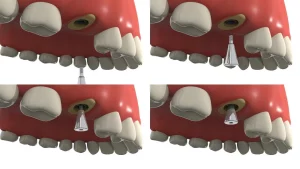
- Strict Disinfection and Sterilization: All dental instruments should undergo rigorous cleaning, disinfection, and sterilization after use. High-temperature steam sterilization is an effective and commonly used method to eliminate HIV.
- Promotion of Single-Use Instruments: For certain high-risk procedures, using single-use dental instruments is an effective way to reduce infection risks. This not only helps prevent cross-contamination but also ensures that each patient uses clean, sterile tools.
- Enhancing Staff Training and Education: Dental clinics should regularly train staff in infection control and prevention knowledge to improve their professional skills and awareness. This helps ensure that staff can correctly and safely handle instruments, effectively reducing the risk of cross-infection.
- Importance of Personal Protective Equipment: Dentists, assistants, and other staff should always wear gloves, masks, and goggles when treating patients. This not only protects them from viruses like HIV but also creates a safer and more reassuring environment for patients.
Conclusion
Although the survival time of HIV on dental instruments is relatively short, the risk of infection in dental healthcare settings should not be overlooked. By implementing strict disinfection and sterilization measures, promoting the use of single-use instruments, and enhancing training and infection control protocols, dental clinics can effectively reduce the risk of HIV and other viruses spreading, thereby ensuring the health and safety of both patients and healthcare personnel. Regular training and stringent infection control procedures are essential components in maintaining oral health and public safety.