In the dental field, guided bone regeneration (GBR) is a precise surgical technique that focuses on using barrier membranes to stimulate and accelerate new bone formation in areas around a dental implant site or other dental surgery locations with insufficient bone volume. This technique is widely used to treat bone defects of at least 2 millimeters, including split and window-type defects, laying a solid foundation for the restoration of oral health and function. Bone loss or insufficient bone volume is a common feature of various dental and gum diseases, and GBR is designed to address this issue, ensuring that implants can securely integrate into the patient’s jawbone structure.
This article aims to explore several key aspects: the definition of GBR, the conditions and timing for its implementation, an overview of the materials used, its benefits and potential risks, and pre-operative preparation, providing readers with a comprehensive analysis of this advanced dental treatment technology.

What is GBR?
Guided Bone Regeneration (GBR) is an advanced surgical technique designed to promote the growth of new bone tissue to fill and support areas with insufficient bone volume faced by dental implants and other restorative dental surgeries. This technique acts like cement in construction, effectively filling any bone defects in the jawbone and providing a stable support environment for dental implants. Statistics show that over one-third of implant patients may require some degree of GBR surgery to strengthen the bone structure in the implant area. Notably, areas treated with GBR demonstrate similar implant success rates compared to implants placed in ideal natural bone conditions, bringing good news to many patients.
What materials are used for guided bone regeneration?
During the Guided Bone Regeneration (GBR) process, materials used include barrier membranes and bone graft materials, along with various dental instruments. The choice of appropriate materials and instruments should be made based on the patient’s specific situation and surgical requirements.
I. Barrier Membranes
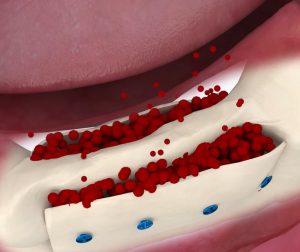
Barrier membranes play a crucial role in GBR by effectively isolating non-bone tissues, such as gums and connective tissues, preventing them from invading the bone graft site. These soft non-osteogenic tissues grow rapidly, while the barrier membrane acts as a shield, creating a stable and safe environment for bone regeneration and allowing slower-growing bone cells enough time and space to fill the defect area.
There are various types of barrier membranes, classified by their material:
- Non-absorbable membranes: Such as titanium mesh and expanded polytetrafluoroethylene (ePTFE) membranes. These membranes provide strong space-maintaining capability but require a secondary surgery for removal, increasing patient discomfort and surgical risk.
- Absorbable membranes: including natural collagen membranes and synthetic membranes. Synthetic membranes offer advantages like large-scale production and repeatability, but their biological efficacy may differ from that of natural materials.
When selecting a barrier membrane, the dentist must consider the patient’s specific situation, surgical needs, and desired postoperative outcomes.
II. Bone Graft Materials
Bone graft materials are another critical component of GBR, primarily used to fill bone defect areas and provide a scaffold that promotes new bone growth. Bone graft materials can be broadly categorized as follows:
- Autogenous bone: Composed of about 30% organic and 70% inorganic components, with 90-95% of the organic component being Type I collagen. Autogenous bone grafts have excellent osteogenic properties and no immune rejection, but they are often rapidly absorbed postoperatively, and the harvesting process may increase patient discomfort and surgical risk.
- Allografts: Allograft materials are obtained from a donor of the same species and stored in bone banks, typically used in forms like fresh frozen bone (FFB), freeze-dried bone allograft (FDBA), or demineralized freeze-dried bone allograft (DFDBA). However, FFB has a high risk of immune response and disease transmission, while the freeze-drying process for FDBA and DFDBA can reduce their immunogenicity.
- Xenografts: Also known as heterologous bone substitutes, these materials come from animal bone or bone-like matrices derived from calcified coral or algae. To avoid immune reactions or disease transmission, the organic components in these materials are usually removed. Bovine cancellous bone is a commonly used animal-derived bone substitute due to its structural similarity to human cancellous bone.
- Synthetic bone: Synthetic bone materials, such as calcium phosphate, bioactive glass, and polymers, offer advantages like large-scale production and customization. However, their biological efficacy may differ from natural bone, and they are generally more expensive.
When selecting bone graft materials, dentists must consider the patient’s specific condition, surgical requirements, material biological properties, safety, and cost-effectiveness.
III. Dental Instruments
In GBR surgery, various dental instruments are also needed to assist in the procedure, such as membrane screws, bone screws and instrument kits, tent pegs, dental curettes, and bone powder. These instruments play important roles during the surgery, including securing the barrier membrane, debriding diseased tissue, and filling bone defect areas.
When is guided bone regeneration needed in dentistry?
Guided Bone Regeneration (GBR) is a technique that utilises the properties of barrier membranes to prevent surrounding soft tissue fibroblasts from entering bone defect areas. This allows osteoblasts at the bone surface sufficient time to proliferate, ultimately achieving tissue regeneration and directed repair. GBR is typically recommended for bone defects of 2 mm or larger and has a wide range of applications in various oral and maxillofacial surgical scenarios. Here are some specific applications:
- Implants dentaires: If there is insufficient bone volume at the implant site after placement, the implant may become exposed. GBR is used here by placing bone graft material on the implant surface and covering it with a membrane to protect the graft, promoting new bone growth and enhancing implant stability. This technique is particularly beneficial for immediate implant placement, as it seals the gap between the implant and extraction site, preventing soft tissue invasion and guiding bone regeneration for osseointegration with the implant.
- Periodontal Disease Treatment: Severe gum disease can lead to bone loss around teeth. GBR can help regenerate the lost bone tissue around teeth, improving periodontal health.
- Trauma Repair: After facial injuries or trauma, GBR can assist in restoring bone structure, promoting the regeneration and repair of facial bones.
- Extraction Prior to Implantation: After tooth extraction, especially in the posterior mandible, GBR can be used to preserve bone for future implant placement. It helps maintain adequate bone volume and aesthetic foundation at the extraction site, facilitating subsequent implant surgery and restoration.
Additionally, GBR can be employed in procedures such as maxillary sinus floor elevation, osteotomy, and onlay bone grafting, addressing various bone deficiency issues.
GBR is an effective bone augmentation technique with broad applications in oral and maxillofacial surgery, supporting dental implants, periodontal disease treatment, and trauma repair. However, the success of GBR depends on several factors, including the choice of barrier membrane, surgical technique, and the patient’s overall health. Therefore, it should be performed under the guidance of a qualified professional.
Advantages of Guided Bone Regeneration (GBR)
Guided Bone Regeneration (GBR) is a widely used technique in oral surgery aimed at promoting the regeneration and repair of bone tissue. Here are the specific advantages of GBR:
- Increased Implant Success Rate: GBR enhances the success of dental implants by using membranes made from biomaterials (such as collagen or absorbable membranes) on the implant surface or in areas of alveolar bone deficiency. This helps guide and promote the regeneration of autogenous bone tissue, thereby increasing bone volume and improving implant conditions. This leads to greater stability for the implants and reduces the risk of loosening or failure due to insufficient bone volume, providing better support and stability.
- Expanded Indications for Implants: GBR addresses the limitations imposed by insufficient bone volume, allowing patients who were previously unable to receive implants due to bone deficiencies to undergo implantation. This broadens the scope of candidates for dental implants, providing more patients with the possibility of restoration.
- Improved Oral Function: By restoring bone volume, GBR contributes to enhancing chewing and speaking abilities, ultimately improving the patient’s quality of life. This is especially crucial for individuals experiencing tooth loss or bone resorption due to periodontal disease.
- Prevention of Further Bone Loss: GBR not only regenerates bone but also helps prevent additional bone loss and related complications. This is significant for maintaining oral health and overall well-being.
- Personalized Treatment Plans: GBR is suitable for various oral conditions, including insufficient bone volume, periodontal disease, and thin or fractured alveolar bone. Dentists can create tailored treatment plans based on individual patient conditions, addressing diverse needs effectively.
- Promotion of Natural Bone Growth: GBR utilizes barrier membranes to create a protected environment that allows osteoblasts to preferentially access the defect area, facilitating natural bone growth. This supports the restoration of alveolar bone height and width, setting the stage for successful subsequent implant or restoration procedures.
Risks Associated with Guided Bone Regeneration (GBR)
Guided Bone Regeneration (GBR) is a valuable technique in dental surgery, but it does come with potential risks that can vary based on individual differences, surgical procedures, and post-operative care. Here’s a detailed overview of the risks associated with GBR:
- Infection:
Post-operative infection is one of the most common complications of GBR. The surgical environment in the mouth is inherently bacterial, and maintaining proper oral hygiene after surgery can be challenging. If an infection occurs, it may be necessary to remove the membrane and any transplanted bone tissue, perform debridement, and delay any further bone grafting and membrane application for 4 to 6 weeks. - Soft Tissue Flap Dehiscence and Membrane Exposure:
Difficulty in closing soft tissue flaps can lead to flap dehiscence after GBR, resulting in membrane exposure and an increased risk of infection. Membrane exposure can negatively impact the healing of the bone defect and increase the chances of surgical failure. - Insufficient Bone Formation:
In some cases, despite undergoing GBR, the amount of new bone generated may be inadequate, leading to suboptimal surgical outcomes. This might necessitate reconsideration of GBR or the application of other bone augmentation techniques to repair the bone defect. - Pain and Swelling:
Post-operative pain and swelling are common reactions following GBR surgery. Pain is usually manageable with pain relievers and ice packs, while swelling may take some time to subside. - Material Rejection:
Although high-quality, biocompatible materials are used to minimize rejection reactions, there is a rare chance that the body may reject the materials used for membranes or bone grafts. If rejection occurs, removal of the grafts and appropriate treatment may be required. - Surgical Failure:
While GBR is effective in most cases, surgical failure can occur due to a combination of factors such as infection, soft tissue flap dehiscence, and insufficient bone generation. Failed surgeries may require additional procedures to repair or reconstruct the bone defect. - Other Complications:
Beyond the risks mentioned, GBR surgery may also lead to other complications, including post-operative bleeding, nerve damage, or injury to adjacent teeth. The incidence and severity of these complications can vary among individuals, but careful surgical technique and post-operative care can help mitigate these risks.
To reduce the risks associated with GBR, patients should undergo a comprehensive oral examination and assessment prior to surgery to ensure appropriate indications for the procedure. Post-operative care is also crucial, including maintaining oral hygiene, avoiding strenuous activities, and attending follow-up appointments. Any discomfort or complications should be promptly addressed with medical consultation and treatment.
Guided Bone Regeneration (GBR) Surgical Process
The surgical process for Guided Bone Regeneration (GBR) typically includes several key steps:
1. Preoperative Preparation
- Oral Hygiene: Rinse the mouth with 0.12% chlorhexidine three times for 30 seconds each to clean the oral cavity and reduce the risk of infection.
- Medication: Administer antibiotics and pain relievers to prevent infection and alleviate post-operative pain.
- Patient Assessment: Conduct a comprehensive oral examination to ensure the patient is suitable for GBR surgery.
2. Surgical Incision and Soft Tissue Flap
- Local Anesthesia: Apply local anesthesia to the surgical area to minimize pain and discomfort for the patient.
- Incision: Make a 2-3 mm horizontal incision on the palatal side of the alveolar ridge, with vertical incisions towards the buccal side at both the mesial and distal ends.
- Flap Elevation: Elevate a full-thickness soft tissue flap, clearing residual soft tissue from the bone surface to adequately expose the implant site.
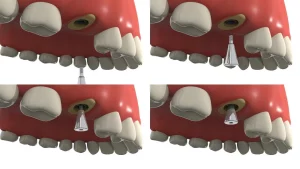
3. Implant Placement
- Observation and Measurement: Assess and measure the condition of the local alveolar bone to ensure it meets the requirements for implant placement.
- Sequential Drilling: Follow surgical principles to prepare the implant site step by step.
- Implant Insertion: Insert the implant, ensuring that each implant achieves good initial stability.
4. Measurement and Bone Grafting
- Measure Bone Defect: Assess the size and extent of the bone defect surrounding the implant.
- Drilling: Create small perforations on the surrounding bone surface with a small round bur to encourage bleeding and facilitate bone formation.
- Greffe osseuse: Fill the space beneath the membrane with autogenous bone fragments or synthetic bone graft materials to prevent membrane collapse and maintain the space for bone regeneration. Autogenous bone can be sourced from the surrounding implant area or other donor sites.
5. Membrane Placement and Fixation
- Select Membrane: Choose an appropriate membrane based on the size of the bone defect and trim it as necessary.
- Shaping the Membrane: For non-resorbable titanium membranes, use a shaping instrument to achieve the desired form, ensuring the edges extend at least 2-3 mm beyond the defect margins and remain 12 mm from adjacent teeth.
- Fix the Membrane: Resorbable membranes can be secured with sutures, caps on the implant, and membrane pins; titanium membranes are fixed with caps and 4-6 membrane pins.
6. Closure of Soft Tissue without Tension
- Trim Flap: Cut the soft tissue flap at appropriate locations.
- Suture: Suture the periosteum and mucosal flap in a tension-free manner, using a combination of mattress and interrupted sutures to close the surgical site.
7. Postoperative Care and Follow-up
- Prevent Infection: Continue antibiotics for one week post-surgery and use chlorhexidine mouth rinse three times daily for two weeks.
- Use of Dentures: Avoid wearing dentures for two weeks post-surgery; after this period, dentures can be used if they adequately cushion and cover the implant area.
- Regular Follow-up: Schedule regular follow-ups, with the second-stage implant surgery occurring 6-8 months post-surgery.
Throughout the surgical process, the surgeon must strictly adhere to aseptic techniques to ensure the cleanliness and sterilization of surgical instruments and materials. Additionally, patients should actively cooperate with their doctor’s instructions and advice to ensure effective preoperative preparation and postoperative care.
Conclusion
Guided Bone Regeneration (GBR) technology holds significant value in modern dentistry, offering new treatment options for patients who struggle with insufficient bone volume for dental implants and other restorative procedures. By promoting the regeneration of bone tissue, GBR not only helps restore oral function but also enhances aesthetics, ultimately improving patients’ quality of life.
Although GBR surgery carries certain risks, such as infection, surgical failure, pain, and swelling, these risks are generally manageable. Through meticulous surgical techniques, effective postoperative care, and active patient cooperation, these risks can be significantly reduced. In cases of substantial bone defects, the potential benefits of GBR technology often far outweigh its risks.
Thus, for dental patients who are suitable candidates for GBR technology, it represents a treatment option worth considering. Every patient’s situation is unique, making it crucial to consult a professional dentist before deciding on GBR technology. The dentist will assess the suitability of GBR based on the patient’s specific circumstances, including oral health status, medical history, and individual needs, providing personalized treatment recommendations.
Overall, guided bone regeneration technology offers new hope for patients facing restoration challenges due to insufficient bone volume. With proper diagnosis and treatment, GBR can help patients regain oral health and enhance their quality of life.