Introduction to Guided Bone Regeneration (GBR)
Guided Bone Regeneration (GBR) is a crucial dental technique designed to promote the formation of new bone by creating a biological barrier in areas of bone defects. This technique uses specific barrier membranes to isolate soft tissue cells (such as epithelial and fibroblast cells) from the bone defect area, thereby preventing interference with the bone-forming process. The primary goal of GBR is to create and maintain space for bone graft materials while allowing oxygen and nutrients to reach the grafted site, facilitating bone tissue regeneration. This technology holds significant clinical value in periodontal treatment and dental implantology, effectively enhancing patients’ oral health.
Historical Development and Evolution of GBR Technology
The origins of GBR technology can be traced back to the 1980s, when Dahlin et al. introduced the concept of guided tissue regeneration (GTR), which later evolved into GBR technology. As research progressed, GBR became widely applied in dentistry, particularly for addressing periodontal defects and bone loss around implants. In recent years, advancements in biomaterial science have led to the development of various innovative barrier membranes, providing higher predictability and reducing the risk of complications for GBR procedures.
The Biological Principles of GBR
The biological principles of GBR are based on the differences in proliferation rates of various cell types in tissue defects. Typically, fibroblasts and epithelial cells migrate much faster than bone-forming cells. Without effective isolation of these cells, bone-forming cells may be inhibited during the bone repair process. By using either resorbable or non-resorbable barrier membranes, GBR establishes a sealed space in the defect area to prevent the migration of soft tissue cells. This allows sufficient time and space for bone-forming cells to proliferate and differentiate. This method not only facilitates the formation of new bone but also improves the quality of bone regeneration.
Indications for Guided Bone Regeneration (GBR)
Guided Bone Regeneration (GBR) is a widely used technique in the field of dentistry, primarily aimed at addressing issues of bone defects and insufficient bone volume. Below is a detailed overview of the indications and contraindications for GBR.
Indications
- Preservation of Alveolar Ridge After Tooth Extraction
After tooth extraction, the alveolar bone resorbs rapidly, which can complicate future implant placement. GBR can effectively preserve bone volume at the extraction site, slowing the resorption process and creating favorable conditions for subsequent implant procedures. - Localized Bone Defects or Insufficient Bone Volume Before Implant Surgery
If localized defects or insufficient bone volume are detected in the alveolar bone before implant surgery, GBR can enhance implant stability by promoting new bone formation. - Bone Defects Around Implants During Surgery
During implant surgery, GBR technology can be used to restore bone tissue in areas where bone defects are observed around the implant, thereby increasing the success rate of the procedure. - Bone Defects Caused by Peri-Implantitis
For bone defects at the neck of implants caused by peri-implantitis, GBR can effectively repair the damaged area and restore its structure and function.
Contraindications
- Poor General Health
Patients with severe systemic diseases such as uncontrolled diabetes, heart disease, or hypertension may not tolerate surgery. These conditions are generally considered contraindications for GBR procedures. - Local Infection or Inflammation
If there is acute or chronic inflammation in the local area, such as periodontitis in adjacent teeth, these issues should be treated before proceeding with GBR to ensure a clean and safe surgical environment. - Poor Oral Hygiene
Patients who are unable to maintain good oral hygiene (e.g., plaque control index exceeding 20%) are not suitable for GBR, as this increases the risk of infection and compromises healing outcomes. - Local Tissue Lesions
Significant gingival and mucosal lesions in the local area may affect the surgical outcome. These issues should be addressed before considering GBR.
Materials Used in Guided Bone Regeneration (GBR)
Guided Bone Regeneration (GBR) plays a significant role in dentistry and bone tissue engineering, with its success closely tied to the materials used. The primary materials for GBR include barrier membranes and bone graft substitutes. Below is a detailed overview of these materials.
Barrier Membranes
Barrier membranes are a core component of GBR, designed to prevent non-osteogenic cells (such as fibroblasts and epithelial cells) from entering the bone defect area, ensuring an uninterrupted bone regeneration process. Based on their absorbability, barrier membranes are classified into two types:
- Absorbable Membranes
These membranes degrade gradually in the body and are typically made from biocompatible materials such as collagen, polylactic acid (PLA), or polyglycolic acid (PGA). Their key advantage is that they do not require a second surgery for removal and are gradually replaced by new tissue during healing. However, their degradation rate and mechanical strength can impact their ability to provide initial support during the early stages of healing. - Non-Absorbable Membranes
These membranes, often made from polytetrafluoroethylene (PTFE) or other synthetic materials, offer superior mechanical strength and stability. They provide long-term support but require surgical removal after healing. Non-absorbable membranes are particularly effective in preventing soft tissue cell invasion.
When selecting a barrier membrane, clinicians consider the patient’s specific condition, defect type, and expected healing time to determine the most suitable membrane type.
Bone Grafts and Substitutes
Bone grafts or substitutes are often required to fill defect areas during GBR procedures. Based on their source and nature, bone graft materials can be categorized as follows:
- Autografts
Autologous bone is harvested from the patient’s own body and typically offers the best biocompatibility and osteogenic potential. However, autografts require an additional surgical site, which may lead to postoperative pain and complications. - Allografts
Allogenic bone is sourced from human donors and undergoes rigorous processing to remove immunogenic components. It offers good biocompatibility without the need for an additional surgical site but carries a potential risk of immune rejection. - Xenografts
Xenogenic bone, commonly derived from animals (e.g., bovine or porcine sources), is treated to remove immunogenic components. While these materials are relatively accessible, their biocompatibility and osteogenic potential may be inferior to autografts or allografts. - Synthetic Substitutes
Synthetic materials include ceramic-based substances such as hydroxyapatite (HA) and beta-tricalcium phosphate (β-TCP), which promote new bone formation and have excellent bioactivity. These materials are often used to fill defect areas but may lack sufficient mechanical strength.
Each type of bone graft or substitute has its own advantages and limitations. When choosing the appropriate material, clinicians take into account the patient’s specific condition, defect characteristics, and expected treatment outcomes to ensure optimal clinical results.
Surgical Techniques in Guided Bone Regeneration (GBR)
Guided Bone Regeneration (GBR) is a surgical technique used to repair bone defects, relying on a series of precise steps and methods for successful implementation. Below is an overview of the surgical techniques involved in GBR, including flap design, membrane placement and fixation, and strategies to ensure primary closure and wound stability.
Step-by-Step Procedure Overview
- Preoperative Assessment
Before surgery, the clinician conducts a comprehensive oral examination and imaging evaluation to determine the type and extent of the bone defect and to formulate an individualized surgical plan. - Anesthesia
Depending on the patient’s needs, local or general anesthesia is administered to ensure comfort throughout the procedure. - Flap Design
In the surgical area, the clinician designs an appropriate soft tissue flap based on the location and size of the defect. The flap should be sufficiently large to cover the defect after surgery and ensure adequate blood supply. - Bone Defect Debridement
After exposing the bone tissue, the clinician cleans the defect area, removing any necrotic or infected tissue to prepare for subsequent grafting and membrane placement. - Membrane Placement
A suitable barrier membrane (absorbable or non-absorbable) is selected and placed over the bone defect. The membrane must fully cover the defect and avoid direct contact with surrounding soft tissue. - Membrane Fixation
Depending on the membrane type, specific fixation methods such as titanium pins, membrane tacks, or sutures are used to secure the membrane in place, preventing displacement or collapse. This step is crucial for maintaining the biological barrier beneath the membrane. - Filling Bone Graft Materials
Bone graft materials, including autografts, allografts, xenografts, or synthetic substitutes, are placed beneath the membrane to promote new bone formation. - Suturing and Closure
After completing the procedure, the clinician carefully sutures the flap to ensure tight and tension-free wound closure, which promotes healing. Techniques such as mattress sutures and interrupted sutures are used to maintain wound stability effectively.
Ensuring Primary Closure and Wound Stability
To ensure primary closure and stability of the wound postoperatively, clinicians adopt the following measures:
- Proper Alignment
During suturing, ensure that the soft tissue flap is properly aligned to cover the membrane and graft materials without excessive tension. - Tension-Relieving Incisions
If the graft volume is significant and closure is difficult, tension-relieving incisions may be performed to reduce tension on the flap. This involves releasing less mobile tissues, allowing the flap to better adapt to the membrane. - Postoperative Monitoring
Regular postoperative follow-ups are necessary to monitor wound healing and check for complications such as infection or membrane exposure. If issues arise, timely measures such as enhanced local disinfection or debridement may be required.
By following these steps and techniques, GBR can effectively promote bone regeneration, providing better treatment outcomes for patients. Surgeons must maintain a high level of attention at every step to ensure surgical success and minimize the risk of complications.
Clinical Applications of Guided Bone Regeneration (GBR)
Guided Bone Regeneration (GBR) has broad clinical applications in dentistry, particularly in addressing bone defects and improving bone quality around dental implants. Below are the primary clinical applications of GBR, including ridge augmentation for dental implants, management of peri-implant defects, and post-extraction socket preservation.
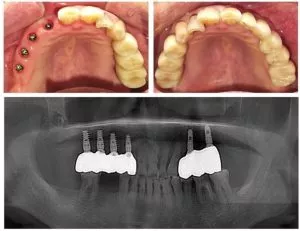
1. Ridge Augmentation for Dental Implants
Ridge augmentation is a key application of GBR, aimed at increasing the height and width of the alveolar bone to provide sufficient support for dental implants. In many cases, patients requiring implant surgery may have inadequate alveolar bone to meet implantation requirements. Using GBR, clinicians can place suitable bone substitute materials in the defect area and apply a barrier membrane to prevent soft tissue cells from interfering with the bone formation process. This approach effectively promotes new bone growth, creating favorable conditions for subsequent implant placement and improving implant success rates.
2. Management of Peri-Implant Defects
GBR in dentistry is equally important in the treatment of bone defects surrounding already implanted dental implants. In such cases, GBR can be applied to the defect area using biomaterials and barrier membranes to promote new bone formation. Research has demonstrated that GBR significantly improves bone quality around implants, thereby reducing the risk of implant failure. With regular monitoring and appropriate postoperative care, patients can achieve good healing outcomes and long-term stability.
3. Socket Preservation Following Tooth Extraction
After tooth extraction, patients often face irreversible bone resorption, which can complicate future implant or restorative treatments. GBR plays a vital role in post-extraction socket preservation. By immediately placing biomaterials in the extraction socket and covering them with a barrier membrane, GBR effectively minimizes bone loss and promotes new bone growth. This process not only helps maintain the morphology of the extraction site but also provides sufficient bone volume for subsequent implant placement. Studies have shown that socket preservation using GBR significantly increases the success rate of future implant treatments.
Guided Bone Regeneration (GBR) is a versatile and effective technique with extensive clinical applications in dentistry. Whether for ridge augmentation, peri-implant defect management, or post-extraction socket preservation, GBR can significantly enhance oral health and treatment outcomes. By leveraging this technology, clinicians can offer better treatment options and improve patients’ quality of life.
Complications and Management in Guided Bone Regeneration (GBR)
Although Guided Bone Regeneration (GBR) offers significant advantages in dental applications, it is not without potential complications. Understanding these complications and their management strategies is crucial for ensuring successful outcomes.
Common Complications
- Membrane Exposure
Membrane exposure is the most common postoperative complication in GBR. It can be categorized into four levels:- Grade I: Small exposure (≤3 mm), without purulent exudate.
- Grade II: Large exposure (≥3 mm), without purulent exudate.
- Grade III: Exposure with purulent exudate.
- Grade IV: Abscess formation without membrane exposure.
- Infection
Postoperative infection can arise from membrane exposure or poor oral hygiene before or after the procedure. Infection triggers inflammation, delays healing, and may require additional interventions. - Soft Tissue Injury
Soft tissue perforation or tearing may occur during surgery, potentially affecting the outcome and causing patient discomfort. - Neurological Complications
In some cases, patients may experience altered or reduced sensation, such as numbness, due to nerve involvement during the procedure.
Prevention and Effective Management Strategies
1. Preoperative Preparation
- Conduct a thorough oral examination to rule out any potential infections or issues.
- Emphasize excellent oral hygiene to minimize postoperative infection risks.
2. Selection of Appropriate Materials
- Choose barrier membranes (resorbable or non-resorbable) based on the patient’s specific needs to reduce the risk of membrane exposure.
- Use materials with high biocompatibility and mechanical strength to enhance membrane stability.
3. Postoperative Care
- Advise patients to follow meticulous oral hygiene practices and use antimicrobial mouthwash, such as chlorhexidine, to lower bacterial infection risks.
- Schedule regular follow-ups to monitor wound healing and promptly address any abnormalities.
4. Management of Membrane Exposure
- Grade I Exposure: Treat with topical chlorhexidine gel and monitor for healing progress.
- Grade II or Higher Exposure: If accompanied by purulent exudate or infection, consider removing the exposed portion and performing tension-free suturing to promote healing.
- Severe Cases (e.g., Grade III/IV): Immediately remove the implant, bone substitute materials, and barrier membrane. Administer systemic antibiotics to control infection and stabilize the patient’s condition.
While GBR complications such as membrane exposure, infection, and soft tissue or neurological issues can occur, proper preventive measures and timely management significantly reduce risks. By selecting suitable materials, ensuring rigorous surgical techniques, and providing comprehensive postoperative care, clinicians can enhance the success rates of GBR procedures and improve patient outcomes.
Latest Advances and Future Directions
Guided Bone Regeneration (GBR) technology continues to evolve in the fields of dentistry and bone tissue engineering, with innovations in materials and techniques opening up new possibilities. Below is an overview of the latest developments and future directions in GBR.
Innovations in Materials and Techniques
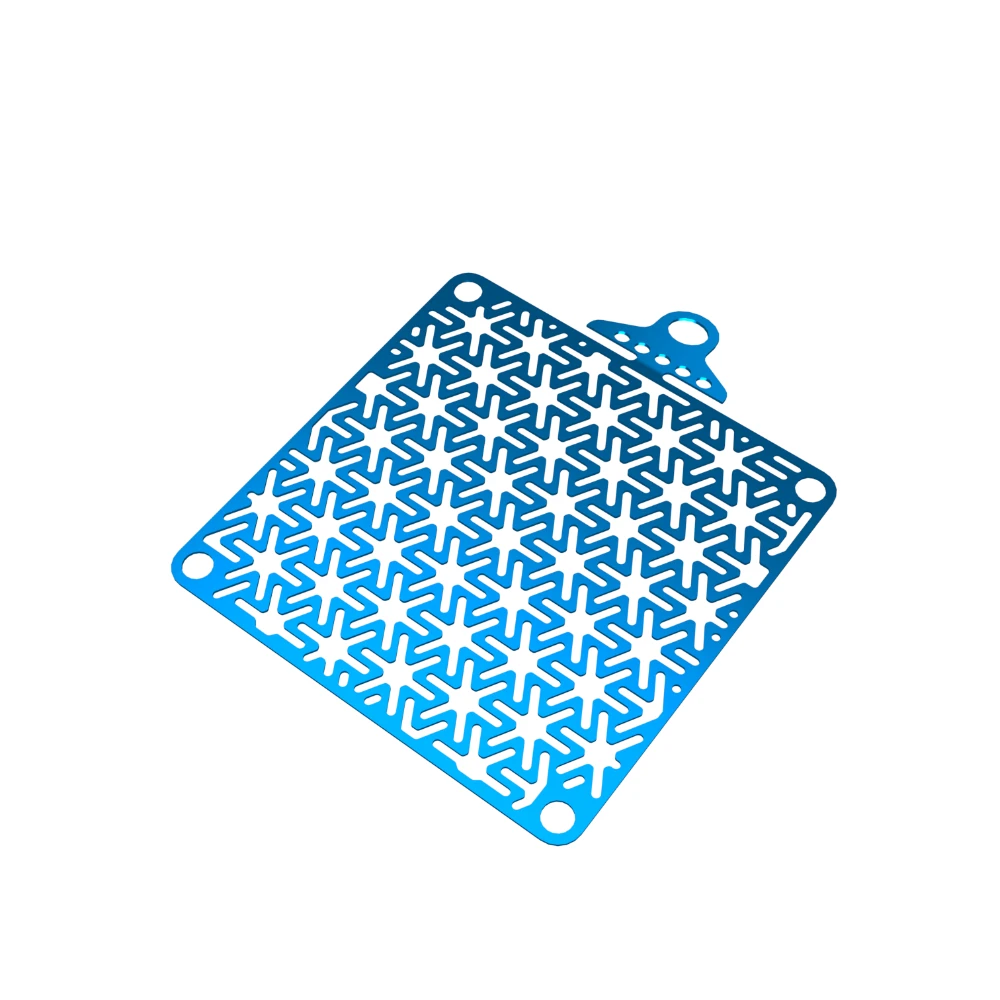
- Novel Barrier Membrane Materials
- Titanium Carbide Thin Film:
A research team from Peking University School of Stomatology and Beihang University has developed a high-strength self-supporting titanium carbide thin film with the following characteristics:- Excellent mechanical strength, providing long-term support in bone defect areas.
- The ability to effectively eliminate reactive oxygen and nitrogen species, improving the bone regeneration microenvironment.
- Promotion of M2 macrophage polarization to enhance bone tissue regeneration.
This innovation addresses the shortcomings of traditional GBR membranes in bone regeneration and paves the way for future clinical applications【1】.
- Titanium Carbide Thin Film:
- Functionally Graded GBR Membranes
- Gradient Structures and Functional Design:
Researchers are exploring composite membranes with gradient spatial structures and multifunctional properties to meet the diverse needs of GBR procedures. These membranes:- Prevent non-osteogenic cells from infiltrating the bone defect area.
- Possess antibacterial and osteogenic properties.
- Significantly improve bone regeneration outcomes【4】.
- Gradient Structures and Functional Design:
- Biodegradable Magnesium-Based Metal Membranes
- Biodegradable Magnesium Materials:
Magnesium-based biodegradable guided bone regeneration membranes are emerging as a promising alternative to traditional materials due to their:- Excellent mechanical properties.
- Superior biocompatibility.
- Enhanced osteogenic performance.
These materials have achieved significant progress in basic and translational research, offering ideal solutions for treating maxillofacial bone defects【3】.
- Biodegradable Magnesium Materials:
Ongoing Research and Future Potential
- Integration of Diverse Materials
Future research is likely to focus on combining various types of biomaterials, such as nanoparticles, nanofibers, and three-dimensional scaffolds, to further enhance the performance of GBR membranes. This multifaceted approach is expected to improve the antibacterial, osteogenic, and biocompatible properties of the membranes【2】【4】. - Personalized Treatment Plans
With advancements in biomaterial science, personalized treatment is becoming increasingly feasible. Tailoring GBR solutions to meet the specific needs of individual patients will improve treatment outcomes. - Clinical Translational Research
As new materials and techniques emerge, their clinical application will be a key focus. Collaboration between researchers and clinicians will be essential to ensure the efficacy and safety of these materials in practice【5】. - Long-Term Monitoring and Evaluation
Long-term follow-up and evaluation of new technologies and materials will become increasingly important. By collecting clinical data, treatment protocols can be continuously optimized, ultimately enhancing patient satisfaction.
Conclusion
Guided Bone Regeneration (GBR) technology provides an effective solution for addressing bone defects in the field of dentistry. By utilizing barrier membranes, GBR creates a biological barrier in bone defect areas, preventing interference from non-osteogenic cells and promoting the proliferation of osteogenic cells and the regeneration of bone tissue. This technique not only increases the success rate of dental implants but also offers new possibilities for periodontal treatment and alveolar bone reconstruction.
The introduction of GBR technology has significantly enhanced the outcomes of dental treatments, making implant surgeries viable for patients previously deemed ineligible due to insufficient bone volume. By effectively promoting bone regeneration, GBR improves the stability of implants while enhancing patients’ oral functionality and aesthetics. Moreover, advancements in materials and techniques have further improved the success rates and predictability of GBR in clinical applications.
In summary, GBR, as a crucial bone regeneration technology, plays an indispensable role in enhancing dental treatment outcomes and improving patients’ quality of life. In the future, with continued research in material science and bioengineering, GBR is expected to be further optimized, providing safe and efficient treatment options for more patients.