Dental implants, as an advanced tooth restoration technology, effectively replace missing teeth and restore both the function and aesthetics of the mouth. Although the use of dental implants in the UK is somewhat lower compared to other European countries, their popularity is rapidly increasing, with the dental implant industry in the UK experiencing a significant growth of 20% to 30% in recent years.
This article will delve into key aspects of dental implants, including their definition, lifespan, factors influencing their longevity, and methods for extending their lifespan. It is important to note that dental implant surgeries are typically performed in private medical institutions, and may not be suitable for patients with certain medical conditions. If you are considering dental implant surgery, our oral and maxillofacial expert consultant team is here to provide you with professional guidance.
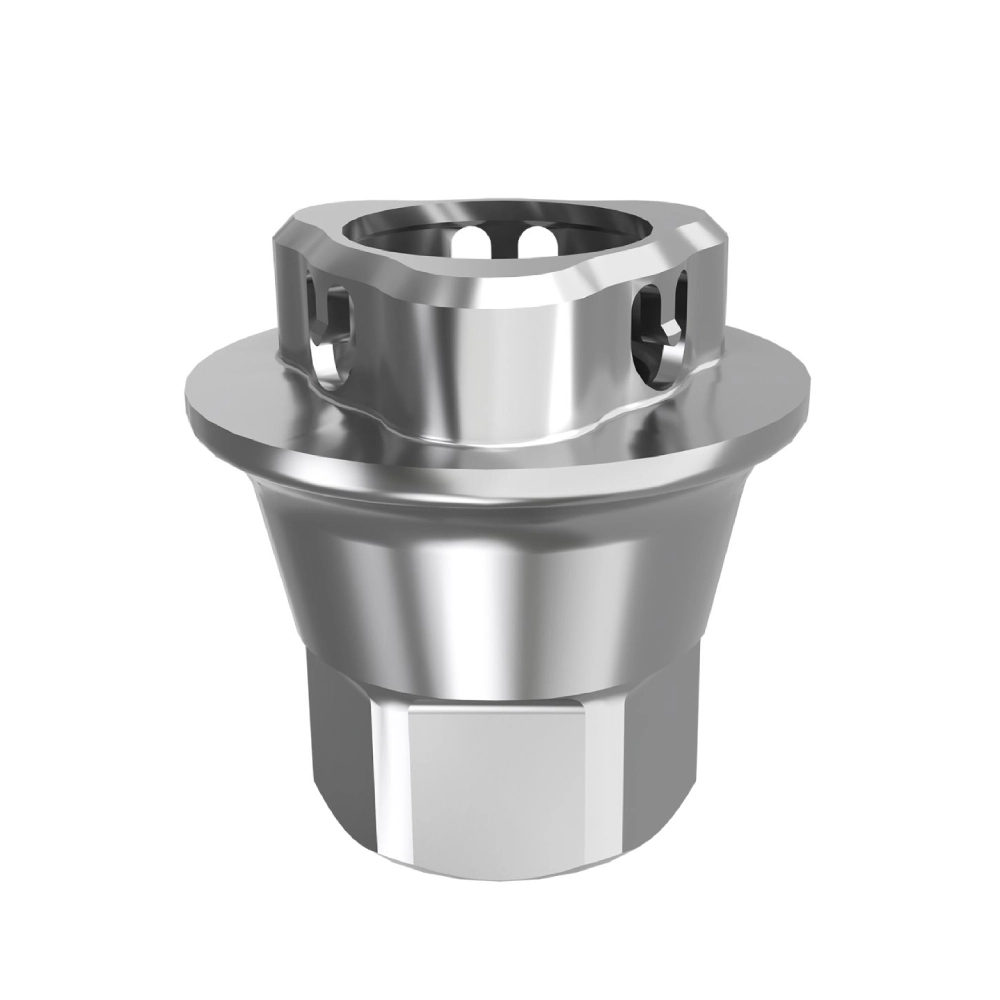
A dental implant is a precise tooth replacement device designed to mimic the structure and function of natural teeth. The implant itself is accurately placed into or onto the jawbone, serving as a stable artificial tooth root. A realistic dental crown is then fixed onto the implant to restore both the appearance and chewing function of the tooth.
Dental implants are typically considered a permanent solution in oral care. According to research, the success rate of dental implants is as high as 90% to 95% over a period of up to 10 years, demonstrating their excellent stability and durability.

What is a dental implant?
Dental implants are an advanced dental restoration technique that involves implanting a titanium screw into the jawbone. This screw acts as an artificial tooth root, providing a stable foundation for the subsequent placement of artificial teeth or dental bridges. Specifically, dental bridges are used to replace two or more missing teeth, while a single crown (artificial tooth) is used to replace an individual missing tooth.
Over time, the implant fuses with the jawbone through a process known as osseointegration, which ensures the stability of the implant. However, some patients may face issues with insufficient bone volume due to trauma, periodontal (gum) disease, or other causes, making it impossible to directly support the implant. Additionally, the bone that once supported the extracted tooth may gradually resorb and dissolve, further exacerbating this problem.
To address this issue, patients may undergo bone augmentation procedures, such as autogenous bone grafting, to add new bone to the upper or lower jaw. This new bone typically comes from other parts of the patient’s body, such as the hip bone or tibia. In addition to autogenous bone grafting, there are alternative bone augmentation methods available, including allografts (using synthetic bone material), xenografts (using animal bone), and alloplastic grafts (using donor-derived human bone). However, these alternative methods often do not perform as effectively as autogenous bone grafting.
Once the graft has fully integrated and healed with the jawbone, it serves as a solid foundation for the titanium implant to securely support the artificial tooth or dental bridge.
Types of Dental Implants
- Endosteal Implants
- Appearance and Material:
Endosteal implants usually resemble small screws or cylindrical shapes. They are primarily made of titanium, but sometimes ceramic can be used as an alternative material. - Procedure:
Endosteal implants are typically inserted into the jawbone in a two-step process. During the surgery, the patient will be given anesthesia to ensure they feel no pain. The surgeon will make an incision in the gum and carefully drill into the jawbone to create a space for the implant. - Healing and Fixation:
After the implant is placed, the jawbone and implant will undergo a healing process called osseointegration. During this period, a metal post called an abutment is typically used to attach the dental crown to the implant. - Indications:
Endosteal implants are suitable for patients who have enough healthy jawbone to support the implant. In some cases, if the jawbone is insufficient, additional procedures such as bone grafting, sinus lift, or ridge expansion may be required to provide a more solid foundation.
- Appearance and Material:
- Subperiosteal Implants
- Appearance and Structure:
Subperiosteal implants are placed under the gum but above the jawbone. They consist of a metal framework with small extensions that slightly protrude from the gum. - Procedure:
The placement of subperiosteal implants is a multi-step process. First, an impression of the jawbone is taken to ensure the implant fits properly. After the area is treated, an incision is made in the gum, and the metal framework of the implant is placed on top of the jawbone. - Indications:
Subperiosteal implants are typically recommended for patients who do not have sufficient healthy jawbone to support endosteal implants. They are also suitable for those who cannot or do not wish to undergo additional surgeries (such as bone grafting). - Subsequent Treatment:
After the implant is placed, a dental crown can be attached to the small protruding extensions of the metal framework during follow-up visits.
- Appearance and Structure:
What is the lifespan of dental implants?
The lifespan of dental implants is a complex and variable topic, but generally, dental implants are designed to be durable and long-lasting restorative solutions. Studies show that 90% to 95% of implants maintain a high success rate within 10 years of implantation. In fact, many dental implants can last 20 years or even longer, providing patients with stable and enduring oral restoration.
It is important to note that while the lifespan of implants is generally long, the dental crown (the artificial tooth part) may have a relatively shorter lifespan. The crown and abutment (the metal post that connects the implant and the crown) are typically placed only after the implant has securely integrated with the jawbone. Because the crown undergoes continuous wear and tear in daily use, its lifespan may be shorter than that of the implant itself. Studies indicate that 50% to 80% of crowns can last 15 to 20 years. However, replacing the crown is relatively simple and cost-effective, so even if replacement is necessary, it does not significantly impact the patient’s overall oral health.
However, the success of dental implants is not guaranteed. Implants may fail within a few months or years due to various reasons. To better understand the lifespan of dental implants, we need to consider factors that may affect their longevity. These factors include, but are not limited to, the patient’s oral hygiene habits, bone density, bite relationship, smoking, and alcohol consumption. By improving these factors, patients can extend the lifespan of their dental implants.
In conclusion, the lifespan of dental implants is a complex issue influenced by multiple factors. While the lifespan of implants and crowns differs, patients can still enjoy long-lasting and stable oral restoration with proper care and maintenance. If you are considering dental implant surgery or have already had implants placed, it is crucial to follow your dentist’s advice, maintain good oral hygiene, and schedule regular oral check-ups and maintenance.
What factors can affect the lifespan of dental implants?
The lifespan of dental implants is influenced by several complex factors, which together determine whether the implant will remain stable and secure in the oral environment over time. Here are some key factors that affect the longevity of dental implants:
1. Bone Quality
The jawbone is the cornerstone for the stability of the implant. If a patient’s jawbone quality is insufficient, or if there are underlying diseases affecting the health of the lower jawbone, the implant may be at risk of failure. Before proceeding with implant surgery, the dentist will conduct a thorough examination of the patient’s jawbone, usually involving X-rays and 3D modeling techniques. If insufficient bone volume is detected, the patient may need additional surgery to augment the bone to ensure the implant has adequate support.
It is important to note that some medical conditions, such as osteoporosis and peri-implant diseases, can gradually weaken the jawbone quality over time. Osteoporosis is a bone disease that causes the bones to become fragile and prone to fractures under mechanical stress. Peri-implant diseases are caused by the accumulation of plaque around the implant, which, if untreated, can develop into peri-implantitis, a condition that threatens the implant’s stability.
2. Peri-implant Diseases
Peri-implant diseases are a significant factor affecting the lifespan of dental implants. These conditions occur when plaque accumulates around the implant. In the early stages, the disease is reversible, but if not properly treated, it can progress into peri-implantitis.
Peri-implantitis is a gum inflammation that severely impacts the stability of the implant and may even lead to implant failure. Therefore, patients must strictly follow the dentist’s oral hygiene instructions after undergoing implant surgery to maintain oral cleanliness and prevent the development of peri-implant diseases.
3. Teeth Grinding (Bruxism)
Teeth grinding is a common oral behavior, where some people unconsciously grind their teeth while sleeping or under stress. This behavior, known as bruxism, can damage dental implants.
The mechanical forces generated during grinding can cause implant screws to loosen or even result in the fracture of the implant, screw, or crown. This is because the repetitive grinding motion can cause slight movement of the implant, disrupting the osseointegration process, which is the tight bond between the implant and the jawbone.
To extend the lifespan of dental implants, patients should avoid grinding their teeth. If bruxism severely affects oral health, the dentist may recommend wearing a mouth guard or undergoing other professional treatments.
4. The Importance of Surgeon Experience
When choosing to undergo dental implant surgery, the experience of the surgeon is critical. Inexperienced surgeons may lead to improper design, poor positioning, or premature installation of the crown, and may even cause damage to oral tissues.
5. Damage to and Protection of Ceramic Crowns
While ceramic crowns are durable, they can still be damaged due to improper use (such as chewing sticky or hard foods, using teeth to open packages, etc.). It is essential to protect both dental implants and natural teeth by avoiding these behaviors.
6. The Impact of Medical Conditions and Medications on Implants
Certain medical conditions (such as cancer, osteoporosis) and medications (such as blood thinners, immunosuppressants) can affect the lifespan of dental implants. People with diabetes also face an increased risk of implant failure.
7. The Type and Position of the Replaced Teeth
The type of teeth being replaced and their location in the mouth can also influence the longevity of the implant. Teeth in the back of the mouth endure more frequent pressure during chewing, so their implants may have a shorter lifespan.
8. Age Factor
Compared to younger individuals, older adults may have a higher risk of implant failure, partly because their healing process tends to be slower.
How to Maximize the Lifespan of Dental Implants
To ensure the longevity of your dental implants, it’s essential to adopt a series of preventive measures and daily care practices. While some factors (like age) can’t be changed, the following recommendations can significantly improve the lifespan of your implants.
1. Avoid Smoking and Excessive Alcohol Consumption
Smoking and excessive alcohol consumption are two major threats to the lifespan of dental implants. Smoking increases the risk of bacterial plaque accumulation around the implant, which can lead to peri-implantitis. Additionally, smoking reduces the oxygen levels in the blood, slowing down the body’s healing process and increasing the risk of gum infections. It is recommended to quit smoking before and after the surgery to lower the risk of infection at the surgical site.
Equally important, avoid consuming alcohol for at least 72 hours after the implant surgery. Alcohol can dilute the blood, potentially affecting the formation of the necessary blood clot in the gums, which is crucial for healing. Excessive drinking can also lead to dehydration, which can hinder recovery at various stages.
2. Maintain Good Oral Hygiene
Dental implants require the same level of care as natural teeth. Although the titanium root and ceramic crown of implants are corrosion-resistant, the surrounding teeth and gums are still vulnerable to damage. Once implants are placed, you must remain vigilant against gum disease, which can lead to implant failure.
To ensure the longevity of your implants, good oral hygiene is vital. Brush your teeth at least twice a day and use dental floss to clean between your teeth to improve gum health and reduce plaque buildup. These steps not only protect your dental implants but also help prevent damage to other teeth, reducing the need for future implants.
3. Regular Dental Checkups
If you have undergone dental implant surgery, regular visits to the dentist are essential. The dentist can detect early signs of gum disease and offer treatment recommendations to ensure the health of your implants. Additionally, they can provide advice on the best practices for maintaining the health of your implant, helping you create a personalized care plan.
It is recommended to visit your dentist every six months for a professional oral examination and cleaning. This will help identify and address any potential issues early, ensuring the long-term stability of your implants.
Comprehensive Strategies for Treating Failed Implants
When inflammation occurs around a dental implant, especially peri-implantitis, immediate removal of the implant may not always be necessary, particularly when there is no significant bone loss in the jaw. In such cases, the key treatment is thorough cleaning of the implant and its surrounding area to eliminate the infection. Doctors typically prescribe antibiotics to help control and heal the infection. The goal during this phase is to restore the health of the implant and prevent the condition from worsening.
However, if the implant fails due to reasons such as uncontrolled infection, severe bone loss, or other factors, removal or replacement of the implant may be considered. This procedure is usually performed under local anesthesia to ensure patient comfort. After the failed implant is removed, the doctor will assess the extent of bone loss. If bone loss is significant, bone graft surgery may be necessary to provide stable support for a replacement implant. Recovery from a bone graft procedure may take several months, during which the patient needs to follow the doctor’s instructions to promote bone regeneration and healing.
In some cases, the failed implant may not be replaced, or the patient may choose not to replace it for personal reasons. In such situations, the doctor will recommend other suitable treatment options based on the patient’s specific circumstances. These alternatives may include the placement of dentures or bridges to restore the patient’s chewing function and oral aesthetics. While these alternatives do not offer the same stability and comfort as dental implants, they can still improve the patient’s quality of life to some extent.
In conclusion, treating failed implants requires a comprehensive approach that takes into account the patient’s specific situation, bone quality, and personal preferences. By employing strategies such as thorough cleaning, antibiotic use, implant removal or replacement, bone grafts, and installation of alternative teeth, doctors can create a personalized treatment plan aimed at achieving the best possible outcome.
Conclusion
Dental implants are an advanced tooth restoration technology that effectively replaces missing teeth, restoring both oral function and aesthetics. Their success rate typically reaches 90% to 95% over a period of 10 years. Factors influencing the lifespan of dental implants include bone quality, peri-implant diseases, teeth grinding habits, the experience of the surgeon, damage to ceramic crowns, medical conditions, and medications. To extend the lifespan of dental implants, patients should maintain good oral hygiene, avoid smoking and excessive alcohol consumption, have regular dental check-ups, and follow the care instructions provided by their dentist. Additionally, if an implant fails, it may require removal, bone grafting, or the use of dentures as alternative treatments. In conclusion, proper care and regular medical follow-ups are crucial for ensuring the long-term stability and success of dental implants.