In this case, we successfully applied the DMDriving 3.5 implant for immediate maxillary anterior implantation, combined with the bone augmentation technique (GBR), to solve the patient’s implantation problem caused by insufficient bone volume. Through precise immediate implantation and bone grafting, the patient achieved rapid recovery after surgery, and restored both beauty and function. This case demonstrates the excellent stability and adaptability of the DMDriving implant, and also reflects our professionalism and technical advantages in complex implant treatment.
Case Information
Basic Information
- Patient Gender: Male
- Patient Age: 59 years old
- Chief Complaint: Loosening of the upper left anterior teeth for several years, now seeking treatment
- Medical History: The patient reports that the upper left anterior teeth have been loose for many years, with no treatment during this period.
- Past Medical History: The patient is generally healthy, with no significant medical history.
- Drug Allergy History: The patient denies any history of drug allergies.
Clinical Examination
Intraoral Examination:
- Mild gingival recession observed throughout the mouth.
- Irregular alignment of the teeth.
- A crossbite between tooth 12 (upper left central incisor) and tooth 22 (upper left lateral incisor).
Condition of the Chief Complained Tooth:
- Tooth 22 (upper left lateral incisor) shows slightly darker discoloration.
- Loosening degree reaches grade III.
- No pain response on percussion (-).
- No signs of inflammation, such as redness, swelling, or purulent discharge, around the gingiva.
- Probing depth of the periodontal pocket is 6mm.
- There is loss of papilla between the mesial and distal gingival papillae.

Radiological Examination
Preoperative Cone Beam Computed Tomography (CBCT) results show:
- The buccal alveolar bone of tooth 21 (upper left central incisor) has been resorbed up to the apical area.
- The palatal alveolar bone has been resorbed up to one-third of the root length.
- A low-density area is observed around the root of tooth 21, which typically suggests the presence of inflammation or bone destruction.
- Additionally, measurements show that the alveolar ridge width is 6.41mm.

Aesthetic risk assessment: Medium risk(ITI Aesthetic Risk Assessment Form ERA)
| Aesthetic Risk Factors | Low | Medium | High |
|---|---|---|---|
| Health Status | Healthy, normal immune function | Light smoking (< 10 cigarettes/day) | Heavy smoking (> 10 cigarettes/day) |
| Smoking Habit | Non-smoker | Moderate | High |
| Patient’s Aesthetic Expectations | Low | Medium | High |
| Lip Line | Low position | Medium position | High position |
| Tooth Biotype | Low arch, thick gingival biotype | Medium arch, thick gingival biotype | High arch, thin gingival biotype |
| Crown Shape | Square | Oval | Pointed |
| Infection Status | None | Chronic | Acute |
| Alveolar Ridge Height | Contact point < 5mm | Contact point 5.5 ~ 6mm | Contact point > 7mm |
| Prosthetic Status | No prosthesis | With prosthesis | With prosthesis |
| Tooth Gap Width | Single tooth > 7mm | Single tooth < 7mm | Two or more teeth |
| Soft Tissue Anatomy | Intact soft tissue | Soft tissue defect | Horizontal bone defect |
| Tooth Malalignment | No bone defect | Non-vertical bone defect | Non-vertical bone defect |
Treatment Plan
Preoperative Planning:
- Preoperative Preparation: One week before the surgery, perform a comprehensive oral maintenance, including cleaning teeth, removing plaque and tartar, etc. Apply chlorhexidine gel locally for disinfection and provide oral hygiene education to the patient to ensure they maintain good oral hygiene postoperatively.
- Blood Preparation: Prior to the surgery, draw the patient’s venous blood to prepare Platelet-Rich Fibrin (PRF), which helps promote wound healing after surgery.
- Minimally Invasive Tooth Extraction: Use minimally invasive techniques to extract damaged or non-retainable teeth, minimizing patient pain and postoperative recovery time.
- Incision Design: Use a trapezoidal incision for better exposure of the surgical area, facilitating implant placement.
- Immediate Implantation: Perform the implant surgery immediately after tooth extraction, implanting DentalMaster brand DMD implants, and combining Guided Bone Regeneration (GBR) technology to promote bone tissue regeneration and implant stability.
- Wound Management: Consider the pros and cons of open healing versus tight suturing. Open healing can reduce the risk of postoperative infection but may prolong the healing time, while tight suturing can speed up healing but may increase the risk of infection. The specific choice depends on the patient’s condition and the doctor’s recommendation.
- Temporary Restoration: Respect the patient’s wishes by not performing temporary restoration. The patient can use existing teeth or dentures for chewing and speaking during the recovery period.
- Routine Restoration: After the implant fuses stably with the bone tissue, carry out routine restorative treatments, such as making crowns or dentures, to restore the patient’s chewing function and appearance.
Detailed Surgical Procedure Record
▲ A #12 sickle-shaped scalpel was used to make an incision along the gingival sulcus of teeth 21, 22, and 23, and an additional vertical incision was made at the mesial of tooth 24.

▲ The mucoperiosteal flap was carefully elevated to expose the buccal alveolar bone of tooth 22, followed by the minimally invasive extraction of tooth 22.

▲ After extraction of tooth 22, the extraction site was scraped to expose the surface of the alveolar bone and open the marrow cavity.

▲ The Soft Tissue Extend technique, which does not involve cutting the periosteum, was used to release soft tissue tension. The original length of the soft tissue flap after elevation was recorded, and a tension comb was used to scrape the soft tissue flap.

▲ Without cutting the periosteum, the soft tissue flap was repeatedly scraped with the tension comb to effectively lengthen the flap. A comparison before and after using the tension comb for expansion showed that the soft tissue flap was extended by 8-9mm without cutting the periosteum.


▲ A ball drill was used for precise localization, followed by stepwise osteotomy preparation. After preparing the site, a Baite DMD NP Ø3.5*11 implant was selected and screwed in, achieving an initial stability of 30N.



▲ The healing abutment was immediately placed.

▲ GBR Procedure: The PRF collagen membrane prepared from the patient’s preoperative venous blood was used, along with bone grafting material mixed with PRF exudate. Bone grafting material was placed at the buccal defect, extending 3-5mm beyond the bone defect and firmly pressed to ensure stability.

▲ The biologic membrane was trimmed and placed over the bone graft area, extending 3-5mm beyond the graft site. A PRF membrane was cross-covered over the surface of the biologic membrane for enhanced protection.

▲ Due to the antimicrobial properties of the biologic membrane and the protective role of PRF, an attempt was made to allow open healing of the extraction site. This helped maintain the gingival papilla in place and preserved the membrane-gingival junction, contributing to better aesthetic outcomes.

▲ Postoperatively, the patient followed routine oral care instructions, rinsed, and took antibiotics for 5 days.

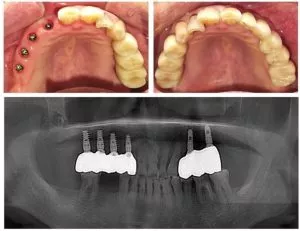
▲ Postoperative CBCT: Excessive bone grafting on the labial side was noted, with the goal of achieving over 2mm of bone regeneration.


▲ Five days postoperatively, the patient returned for suture removal and follow-up due to discomfort caused by the nylon sutures. The gums appeared slightly red and swollen but were clean with no signs of infection. Fibrin was visible over the wound, indicating normal healing.


▲ Chlorhexidine antibacterial gel was applied to the incision area, and the patient was instructed to continue routine mouth rinsing and maintain oral hygiene.

Restoration Process
20 Days Postoperatively: Follow-up appointment shows complete absorption of PRF, with the collagen membrane remaining and clear epithelial coverage.

8 Weeks Postoperatively: Follow-up appointment reveals soft tissue healing with healthy keratinized gingiva.

4.5 Months Postoperatively (Periapical X-ray): ISQ mobility values for the buccal-lingual/mesial-distal directions are 70/73.

4.5 Months Postoperatively (CBCT): CBCT taken to assess progress.

Routine Impression Taken: A standard impression was made.
5 Months Postoperatively: The restoration was completed.

Final Restoration Completed.

Conclusion
This case involves immediate implantation of a single tooth in the aesthetic zone due to a combined dental, pulp, and periodontal condition causing tooth mobility that could not be preserved. The patient had dental malalignment, long-term periodontal and periapical lesions, and was in a Class II extraction site. Oral hygiene was moderate, and the risk of immediate implantation in the aesthetic zone was relatively high. However, a relatively satisfactory implant restoration outcome was ultimately achieved. After a systematic review of this case, the following insights were gained:
- Preoperative Aesthetic Risk Assessment and Radiographic Analysis are the starting point of clinical work. Minimally invasive tooth extraction and standardized surgical procedures, especially accurate three-dimensional placement of the implant and control of initial stability, are key factors for success.
- Soft Tissue Wound Management is crucial for closure. Due to the extraction site, there is often insufficient soft tissue, making wound closure difficult. Additionally, guided bone regeneration usually requires excessive bone grafting, so it is important to adequately release soft tissue tension. In this case, instead of the classic periosteal incision and tension release method, a tension comb was used to achieve an 8-9mm extension of the soft tissue flap, effectively relieving tension while preserving blood supply to the bone graft area from the soft tissue and periosteum. To reduce the risk of wound exposure, a PRF + pig small intestine submucosa (SIS) absorbable biomembrane was used to cover the exposed wound area. SIS biomembranes are more resistant to degradation than conventional collagen membranes, with strong hydrophilicity, elasticity, and some antimicrobial properties, making them suitable for creating conditions for selective “open healing” in the oral environment. This expands the indications for selective open healing of the alveolar ridge preservation wound. “Open healing” allowed for the gingival papilla and membrane-gingival junction to remain in place, laying a foundation for aesthetic outcomes.
- During the Restoration Phase, a personalized impression was used to create a model, and a customized abutment with screw retention was made. This changed the original cross-bite situation of the tooth and was adjusted to a shallow overbite, further enhancing aesthetics. A shortcoming of the case, due to patient factors, was the failure to create an “immediate temporary restoration,” which somewhat affected the improvement of postoperative aesthetics.