In the field of orthodontics, every technological advancement brings new hope and expanded options for patients. With the rapid progress of modern dental medicine, a small yet powerful tool—the orthodontic mini screw—has emerged as a game-changing solution in orthodontic treatment. Acting as a precise “anchor,” this tiny component offers stable and reliable support during tooth movement, enabling orthodontists to design more efficient and personalized treatment plans.
From its initial concept to its widespread clinical adoption today, the orthodontic mini screw has revolutionized traditional orthodontic approaches. Its unique advantages—such as enhanced stability, shorter treatment times, reversibility, and minimally invasive placement—have earned the trust and preference of both orthodontists and patients alike.
Imagine a time when orthodontic treatment required months or even years of adjustments and waiting. Now, with the integration of mini screws, the process has become faster, more predictable, and more effective. Whether it’s closing gaps between teeth, retracting protruding front teeth, distalizing molars, or controlling open bites and deep overbites, mini screws offer new and powerful solutions to some of the most challenging aspects of orthodontics.
Of course, patient concerns like pain management, post-op care, and potential risks are also being addressed through ongoing advancements in technique and technology, making the entire experience safer and more comfortable.
So, how exactly do orthodontic mini screws work? Why are they so critical in modern treatment plans? And what should patients know before deciding to use them? In this article, we’ll explore the fundamentals of orthodontic mini screws—including their definition, benefits, clinical applications, placement procedures, limitations, and how to determine if they’re right for you. By the end, you’ll have a clear, comprehensive understanding of this remarkable innovation and feel more confident in your orthodontic journey.
Introduction to Orthodontic Mini Screws
Orthodontic mini screws, also known as micro-implants or temporary anchorage devices (TADs), are small, screw-shaped components typically fabricated from titanium alloy (Ti-6Al-4V). These devices are utilized in orthodontic treatment to provide stable anchorage points for the application of controlled forces to teeth, thereby enabling precise and predictable tooth movement. Measuring approximately 6 to 10 mm in length and 1.2 to 2.3 mm in diameter, mini screws are inserted into the alveolar bone to serve as fixed anchors, facilitating complex orthodontic movements that are often challenging or unachievable using conventional anchorage methods alone.
The increasing adoption of orthodontic mini screws in contemporary practice is attributed to their exceptional stability, versatility, and minimally invasive nature. Unlike traditional anchorage systems—which typically depend on molars or extraoral appliances—mini screws offer a more reliable and patient-friendly alternative. They are especially effective in cases requiring significant retraction of anterior teeth, space closure, or occlusal correction. Furthermore, their ease of placement, reversibility, and rapid healing time make them a favored option among orthodontists and patients seeking efficient, comfortable, and high-precision treatment.
What Are Orthodontic Mini Screws?
Orthodontic mini screws—also referred to as micro-implants or Temporary Anchorage Devices (TADs)—are small, screw-like implants made from titanium alloy or stainless steel. Designed with a fine-thread structure, these devices typically measure between 6 to 10 mm in length and 1.2 to 2.3 mm in diameter. They are precisely inserted into the jawbone (such as the alveolar bone or zygomatic bone) and serve as stable anchorage points within the orthodontic force system.
These mini screws work through mechanical retention and form a temporary integration with the bone (osseointegration), providing a reliable mechanical anchor. This helps overcome the limitations of traditional anchorage methods, such as headgear or external traction devices.
Key Functions
- Absolute Anchorage Control: By anchoring directly to the jawbone and functioning independently of adjacent teeth, mini screws allow for precise tooth movements—such as retraction of anterior teeth, space closure, and vertical control—without exerting unwanted forces on non-targeted teeth.
- Adaptability for Complex Cases: Ideal for cases where traditional anchorage falls short, such as severe open bites, deep overbites, or extreme crowding.
- Improved Patient Compliance: Unlike conventional appliances that require active patient participation (e.g., headgear), mini screws offer predictable outcomes with minimal dependency on patient compliance, reducing uncertainty during treatment.
Material Characteristics
- Titanium Alloy:
Offers excellent biocompatibility and is relatively soft in texture, making it well-suited for areas with lower bone density, such as the maxilla (upper jaw). Though slightly more expensive and technically complex to place, titanium mini screws are less likely to damage bone tissue and are favored for delicate applications. - Stainless Steel:
Known for its high strength and durability at a lower cost, stainless steel is ideal for areas with higher bone density, such as the mandible (lower jaw). stainless steel mini screws are easy to insert and remove with minimal trauma, making them a popular choice among clinicians.
In modern orthodontics, mini screws are highly valued for their precise biomechanical control, ability to reduce side effects (such as unintended tooth movement), and overall efficiency. As advancements in materials science and minimally invasive techniques continue, the clinical applications of orthodontic mini screws are expanding—solidifying their role as an indispensable tool for delivering effective and individualized orthodontic care.
Key Benefits of Using Orthodontic Mini Screws
Mini screws have become an essential tool in modern orthodontics, enabling complex tooth movements and efficient treatments due to their precise biomechanical control, reduced side effects (such as unwanted tooth movement), and enhanced treatment efficiency.
- Strong Stability (Anchorage Control)
Mini screws are directly inserted into the jawbone, providing an independent anchor point. This avoids applying reactive forces to non-target teeth, allowing for precise tooth movements such as anterior retraction, space closure, and vertical control. They are particularly effective in treating complex cases such as severe open bites and deep overbites. - Shorter Treatment Time
By providing stable anchorage, mini screws accelerate tooth movement, reducing the overall treatment time (for example, shortening the duration for anterior retraction). They also minimize the need for repeated adjustments caused by insufficient anchorage. - Reversibility and Minimally Invasive
The insertion of mini screws causes minimal trauma (with diameters ranging from 1.2 to 2.3 mm) and offers quick recovery. After treatment, they can be easily removed, and the bone tissue typically heals completely without affecting future restorations or implants.
Common Clinical Applications of Orthodontic Mini Screws
Thanks to their precise biomechanical control and minimally invasive nature, orthodontic mini screws are widely used in treating complex cases. By providing independent anchorage, they overcome the limitations of traditional orthodontic techniques, making them especially valuable in the following scenarios:
- Complex Cases: Such as severe open bite, deep overbite, and skeletal protrusion.
- Increased Efficiency: Shortens treatment time and reduces the number of follow-up visits.
- Minimally Invasive and Safe: Small insertion trauma, fast recovery, and high reversibility.
Below are four core clinical applications:
1. Space Closure (Gap Closure)
- Scenario: Required when closing gaps caused by tooth extraction or congenital tooth absence.
- Mechanism: Mini screws act as anchorage points for traction devices (e.g., power chains) that apply force directly to the target teeth, minimizing unwanted tipping of adjacent teeth.
- Advantages:
- Precision: Ensures even closure of spaces while maintaining arch form.
- Efficiency: Reduces treatment duration—gap closure after extractions can be up to 30% faster.
2. Maxillary Anterior Retraction (Improving Facial Profile)
- Scenario: For patients with dental or skeletal protrusion (e.g., bimaxillary protrusion), anterior teeth need to be retracted.
- Mechanism: Screws are placed in the posterior maxilla, serving as anchorage to retract anterior teeth without unwanted mesial movement of posterior teeth.
- Advantages:
- Stable Anchorage: Maintains posterior tooth position to ensure effective anterior retraction.
- Case Versatility: Ideal for patients needing strong anchorage in skeletal protrusion cases.
3. Molar Distalization (Arch Expansion / Bite Adjustment)
- Scenario: Indicated for narrow arches or patients needing posterior bite correction.
- Mechanism: Screws are placed in the buccal cortical bone to apply distalizing forces to molars, expanding the arch or adjusting occlusion.
- Advantages:
- Controlled Movement: Allows isolated molar movement without reciprocal anterior effects.
- Minimally Invasive: Eliminates the need for extraoral devices, enhancing comfort.
4. Open Bite and Deep Overbite Correction
- Scenarios:
- Open Bite: Lack of contact between upper and lower front teeth.
- Deep Overbite: Excessive vertical overlap of the upper front teeth over the lower.
- Mechanism:
- Open Bite: Screws placed in the posterior maxilla intrude anterior teeth, while screws in the posterior mandible upright molars to achieve proper occlusion.
- Deep Overbite: Screws near the maxillary anterior teeth retract and intrude the incisors to reduce the overlap.
- Advantages:
- Multidimensional Control: Allows vertical, horizontal, and sagittal movement.
- Reduced Side Effects: Prevents bite instability caused by over-retraction or molar extrusion typical of traditional methods.
Orthodontic mini screws continue to revolutionize treatment planning and execution by offering unmatched control, efficiency, and adaptability in managing complex dental and skeletal discrepancies.
Placement Procedure and Patient Experience
I. Placement Procedure
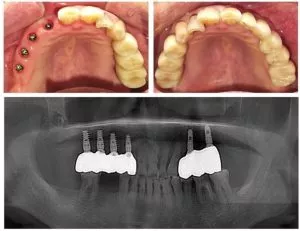
Preoperative Evaluation and Planning
- Imaging Assessment: CBCT or panoramic X-rays are used to evaluate bone density, cortical thickness, and the location of nerves and blood vessels, helping to determine the optimal placement site (e.g., zygomatic-alveolar ridge in the maxilla or the posterior mandibular region).
- Anchorage Planning: Based on treatment goals, mini screw diameter (1.2–2.3 mm) and length (6–10 mm) are selected, along with force direction (e.g., anterior retraction, molar distalization).
Local Anesthesia
- Infiltration Anesthesia: Lidocaine is injected around the insertion site to ensure a painless procedure.
- Anesthesia Confirmation: The procedure begins only after the patient confirms numbness in the area.
Screw Insertion
- Incision and Positioning: No gingival incision is required. A pilot hole (approximately 3–5 mm deep) is drilled using a low-speed handpiece or manual driver at the preplanned site.
- Screw Placement: The screw is slowly inserted along the cortical bone direction to avoid sinus perforation or damage to adjacent roots.
- Stability Test: The screw’s stability is checked by percussion; repositioning may be done if instability is detected.
Post-Insertion Confirmation
- Radiographic Verification: A periapical film or CBCT is taken to confirm the screw’s position relative to nerves and blood vessels.
- Orthodontic Attachment: Traction devices (e.g., elastomeric chains or NiTi springs) are connected to initiate orthodontic force.
II. Pain Management
Intraoperative Pain Control
- Local Anesthesia: Ensures the procedure is completely pain-free.
- Psychological Comfort: Patients are informed about the procedure beforehand to reduce anxiety.
Postoperative Pain Relief
- Immediate Care:
- Cold Compress: Applying ice within the first 24 hours reduces swelling.
- Medication: Taking ibuprofen 30 minutes before surgery significantly decreases postoperative pain.
- Long-Term Management:
- Pain Monitoring (NRS Scale): Pain is assessed at 2, 4, 6, and 8 hours post-op. NSAIDs are prescribed if necessary.
- Mucosal Protection: Orthodontic wax is applied over the screw head to minimize irritation.
Pain Duration
- Initial Phase (1–3 Days): Mild swelling and tenderness; pain typically ≤3 on the NRS.
- Adaptation Phase (1–2 Weeks): Mucosa adapts to the screw, and discomfort usually subsides.
III. Postoperative Care Instructions
Oral Hygiene
- Cleaning Tools: Use a soft-bristle toothbrush, water flosser, or 0.12% chlorhexidine mouthwash to clean around the screw.
- Avoid Irritation: Refrain from using electric toothbrushes within the first 5 days to prevent screw loosening.
Dietary Recommendations
- Food Choices: Avoid hard foods (e.g., nuts, apples); opt for soft foods like porridge and steamed eggs.
- Chewing Technique: Chew using the back teeth to reduce pressure on the screws.
Mucosal Protection
- Covering the Screw: If the screw head causes ulcers, apply orthodontic wax or use a chlorhexidine compound mouth rinse.
- Follow-Up: During checkups, the dentist assesses mucosal healing and adjusts care as needed.
Follow-Ups and Monitoring
- Frequency: Scheduled visits at 1 week, 1 month, and 3 months post-op to assess screw stability and treatment progress.
- Managing Complications:
- Loosening or Dislodgement: Contact the orthodontist immediately; re-insertion may be needed.
- Infection: Signs like redness, swelling, or increased pain may require irrigation and oral antibiotics.
FAQs About Orthodontic Mini Screws
1. Do they hurt?
During the procedure:
Local anesthesia is applied before insertion, so you typically won’t feel significant pain.
In the first few days post-op (1–3 days), you might experience mild swelling or tenderness. Pain levels vary but usually subside within a week.
Post-operative pain management:
You can take over-the-counter NSAIDs like ibuprofen as prescribed by your doctor to relieve discomfort.
Avoid touching the area or chewing hard foods to minimize irritation around the screw site.
2. Can they become loose or fail?
Risk of loosening:
Mini screws have a loosening rate of around 5%–10%. This can occur due to poor insertion positioning, low bone quality, or premature loading.
If a screw becomes loose, contact your orthodontist promptly for evaluation. Re-insertion might be necessary.
Failure management:
Fractures or displacements are rare but may require surgical removal and reassessment of the treatment plan.
3. Do they need to be removed? When?
Is removal necessary?
Yes, mini screws are temporary anchorage devices and need to be removed after treatment is complete.
When to remove them:
They are typically removed 3 to 6 months after insertion, depending on the treatment plan and how the bone heals.
In cases requiring longer treatment, they may stay in place for up to 2 years, but not beyond that in most cases.
Removal process:
Removal is simple and usually doesn’t require anesthesia. Your orthodontist will use a special tool to unscrew and remove it. The bone usually heals completely afterward.
4. Are mini screws suitable for everyone?
Ideal candidates:
Mini screws are suitable for cases requiring strong anchorage, such as retraction of front teeth, molar distalization, or controlling open bites or deep overbites.
They are especially helpful for patients with missing teeth or post-extraction space closure needs.
Not suitable for:
Patients with osteoporosis, underdeveloped jawbones, or existing infections should be carefully evaluated.
Children or adolescents may need assessment based on bone development before use.
Conclusion
As an important innovation in modern orthodontics, orthodontic mini screws provide a breakthrough solution for the treatment of complex malocclusions through their precise anchorage control, minimally invasive nature, and wide range of indications. Clinical research and practice have shown that orthodontic mini screws, by establishing a mechanical system independent of the teeth, significantly improve treatment efficiency in challenging cases such as anterior retraction, molar distalization, and open bite control (e.g., reducing the time to close extraction spaces by 30%), while avoiding the drawbacks of reactive forces on adjacent teeth in traditional treatments, thus achieving more stable orthodontic results.
Their minimally invasive implantation method (no need to cut the gums, only local anesthesia required) and reversible design (can be easily removed after treatment) greatly reduce patient discomfort and postoperative risk. Their high success rate (80%-95%) and low complication rate (loosening rate of approximately 5%-10%) further confirm their clinical reliability.
For patients, orthodontic mini screws not only shorten the treatment duration through precise mechanical control, but also improve treatment comfort through personalized care plans (such as mucosal protection and pain management). However, the application of orthodontic mini screws must follow the principle of individualized assessment, as they are not suitable for all patients. Their effectiveness is influenced by multiple factors, including bone quality, implantation site, and patient compliance.
Therefore, we strongly recommend that patients consult a professional orthodontist before considering orthodontic mini screws, and formulate a scientific and safe treatment plan through comprehensive imaging examinations (such as CBCT) and mechanical analysis. Only in this way can the orthodontic goal of “achieving the greatest aesthetic and functional improvement at the lowest cost” be truly realized, allowing every patient to regain a healthy and confident smile.