Tooth loss not only affects chewing function, speech, and aesthetics but may also lead to long-term complications such as jawbone atrophy and adjacent teeth tilting. However, while traditional dental implants are hailed as the “third set of human teeth,” they require high bone density and surgical tolerance, excluding many patients with insufficient bone volume, advanced age, or sensitivity to surgical procedures. Against this backdrop, mini dental implants, with their revolutionary design and clinical advantages, are gradually emerging as a preferred solution for tooth replacement.
Compared to traditional implants, mini dental implants feature a compact structure with a diameter of only 2-3 mm, overcoming bone volume limitations and achieving stable fixation without the need for complex bone grafting procedures. Their minimally invasive surgical approach (typically performed under local anesthesia with an incision 30% smaller than that of traditional implants) significantly reduces surgical risks, as well as postoperative swelling and pain, making them particularly suitable for patients with osteoporosis, diabetes, or those who fear conventional surgery. Additionally, mini dental implants offer immediate loading and a shorter restoration period (some cases allow for same-day tooth placement), enabling patients to regain confidence in chewing more quickly.
This article will provide an in-depth analysis of the “big potential in a small size” of mini dental implants from multiple perspectives, including technical principles, indications comparison, surgical process differences, and postoperative maintenance. Whether you have been excluded from traditional implants due to insufficient bone volume or seek a more efficient and comfortable tooth replacement solution, this article will reveal how mini dental implants, guided by precision medicine, are redefining the possibilities of tooth restoration.
What Are Dental Implants?
Dental implants are medical devices surgically placed into the jawbone to replace missing tooth roots. Their primary goal is to restore a patient’s chewing function, speech ability, and facial aesthetics while preventing jawbone atrophy and adjacent teeth shifting caused by tooth loss. Below is a comprehensive analysis of dental implants:
Structure and Components
Dental implants typically consist of three main parts:
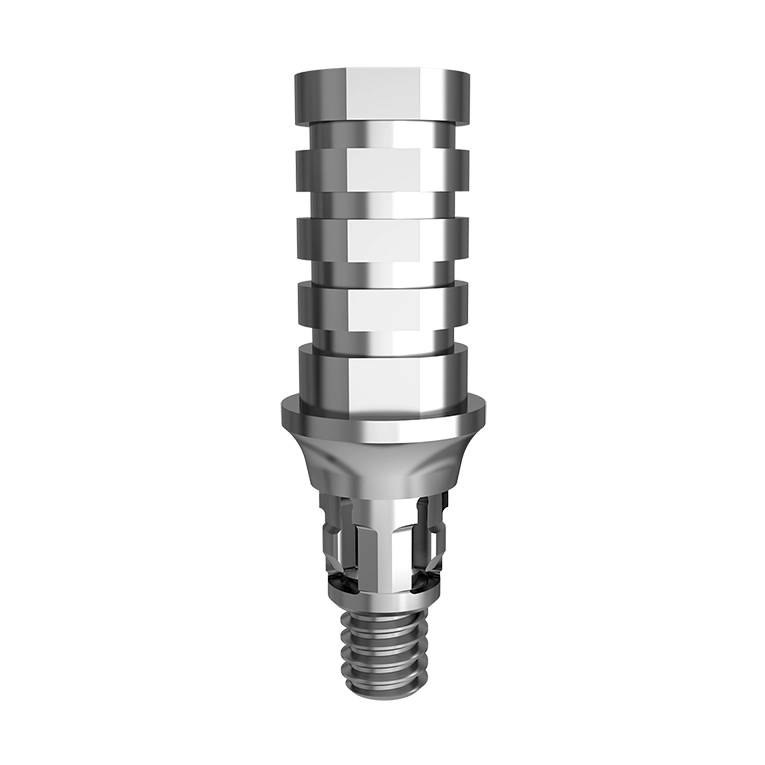
- Implant Fixture – A titanium or titanium alloy screw embedded into the jawbone, acting as an artificial tooth root that integrates with the bone through osseointegration.
- Abutment – A transitional component that connects the implant fixture to the dental crown, extending through the gum and exposed in the oral cavity.
- Crown – A custom-made artificial tooth, available in ceramic, metal-ceramic, or all-ceramic materials, designed to restore the appearance and function of a natural tooth.
Analogy
A dental implant can be compared to a tree: the implant fixture serves as the “roots,” the abutment as the “trunk,” and the crown as the “branches and leaves.” Together, they mimic the structure and function of a natural tooth.
What Are Mini Dental Implants?
Mini dental implants are an innovative oral restoration technology designed to overcome the limitations of traditional implants in cases of insufficient bone volume, low surgical tolerance, or lengthy treatment periods. Their core structure consists of a titanium alloy screw with a diameter of less than 3mm, featuring a spherical end that is directly embedded into the surface of the jawbone, achieving stable fixation without the need for complex flap surgery.
Compared to traditional implants, which require separate placement of the abutment and crown, the integrated design of mini dental implants significantly simplifies the surgical procedure and shortens the treatment period. Additionally, with a much smaller surgical trauma area—only one-third that of conventional procedures—mini dental implants greatly reduce postoperative swelling and pain risks. This makes them an ideal choice for elderly patients, individuals with osteoporosis, or those who fear traditional implant surgery.
Comparison Between Traditional Dental Implants and Mini Dental Implants
Here is the enriched comparison table between traditional dental implants and mini dental implants:
| Dimension | Traditional Implants | Mini Implants |
|---|---|---|
| Diameter | 3.5-6mm | 2-3mm |
| Length | Typically 8-15mm (adjusted based on bone height) | Shorter, usually 4-12mm |
| Material | Mainly titanium alloy, some containing zirconium | Titanium alloy, often with a smoother surface treatment |
| Indications | Suitable for patients with good jawbone conditions and sufficient bone volume | Ideal for patients with low bone volume, alveolar bone resorption, or those needing immediate loading |
| Surgical Trauma | Requires flap surgery, more invasive | Minimally invasive, no flap surgery or only a small incision required |
| Healing Time | 3-6 months (requires time for osseointegration) | Short healing period, some cases allow immediate loading |
| Number of Surgeries | Usually requires 2-3 procedures (implant placement + abutment + crown) | Single-stage surgery, implant and restoration can be completed in one procedure |
| Stability | High (relies on osseointegration, long-term stability) | Moderate (suitable for temporary restorations or low-load areas) |
| Load Capacity | Can withstand significant occlusal forces, suitable for posterior teeth | Limited load capacity, mainly used for anterior teeth or low-load areas |
| Cost | Higher (includes surgical fees, material costs, etc.) | Relatively lower (due to simplified procedures and reduced material costs) |
| Aesthetics | Custom crowns provide excellent aesthetics | Limited crown options but sufficient for basic aesthetic needs |
| Maintenance Difficulty | Requires regular professional cleaning and check-ups | Easier to maintain, but excessive load should be avoided |
| Failure Risk | Low (but failure of osseointegration may require revision surgery) | Slightly higher (as stability depends on local bone conditions) |
| Patient Tolerance | Requires higher surgical tolerance | Minimally invasive, suitable for elderly or medically compromised patients |
Additional Notes:
- The immediate loading feature of mini implants makes them particularly suitable for fully edentulous patients or those who need a quick restoration of chewing function.
- The long-term stability of traditional implants makes them the preferred choice for posterior teeth restoration, but patients must meet the necessary bone conditions.
- Cost variations depend on materials, surgical complexity, and regional factors, requiring case-specific evaluation.
Mini Dental Implant Placement Procedure
Mini Dental Implants (MDIs) are an innovative and minimally invasive solution for missing teeth. Compared to traditional implants, the procedure is significantly simplified, making it particularly suitable for patients with low bone volume, those seeking quick restoration, or those who fear complex surgical procedures. Below is a detailed breakdown of the mini dental implant placement procedure and its key advantages:
1. Preoperative Evaluation and Preparation
- X-ray Examination and Treatment Planning:
The dentist will use panoramic X-rays or CT scans to assess bone density, bone volume distribution, and adjacent structures to determine the optimal implant position and angle. Due to the smaller diameter of mini implants (2-3mm), they require less bone volume than traditional implants, making them an ideal option for patients with bone resorption or osteoporosis. - Local Anesthesia:
The entire procedure is performed under local anesthesia, ensuring the patient remains awake but pain-free.
2. Surgical Procedure: Minimally Invasive, Efficient, and Single-Stage
- Guided Drilling:
The dentist uses a specialized guide drill to create a small hole in the gum tissue (no need for flap surgery). The hole is slightly larger than the implant to ensure precise placement. - Mini Implant Insertion:
A one-piece titanium alloy screw with a ball-shaped tip is inserted into the pre-drilled hole and screwed into the cortical bone. Since mini implants are shorter (4-12mm), the surgical trauma is minimal, and sutures are usually unnecessary. - Immediate Loading (In Some Cases):
If the bone quality at the implant site is sufficient, a temporary crown or O-ring-retained denture can be attached to the implant’s top via a ball-and-socket mechanism, allowing for same-day tooth replacement. Traditional implants, in contrast, require a 3-6 month osseointegration period before loading. - Gum Contouring:
If the implant initially protrudes from the gum, the dentist may slightly adjust the soft tissue around it to ensure a comfortable fit and prevent irritation.
3. Postoperative Care and Precautions
- Dietary Adjustments:
For the first 24-48 hours post-surgery, avoid hard or sticky foods (such as nuts or chewing gum). Instead, opt for soft foods like mashed potatoes and soups to minimize pressure on the surgical site. - Pain Management:
Due to the minimally invasive nature of the procedure, post-surgical pain is typically mild and can be managed with over-the-counter pain relievers. However, if pain persists or worsens, a follow-up visit is necessary to check for infection or implant loosening. - Daily Oral Hygiene:
Use a soft-bristled toothbrush or a water flosser to gently clean around the implant site. Avoid aggressive brushing that may disrupt healing. - Regular Follow-ups:
Follow-up visits are recommended at 1 week, 1 month, and every 6 months to monitor implant stability and gum health.
4. Potential Risks and Contraindications
Risks:
- Initial implant stability may be lower, requiring caution with excessive bite force (e.g., chewing hard foods).
- Poor oral hygiene can lead to peri-implantitis.
Contraindications:
- Uncontrolled diabetes or immune system disorders.
- Heavy smoking (more than 10 cigarettes per day) without willingness to quit.
- Active jaw infections or tumors.
Mini dental implants provide an efficient solution for patients with insufficient bone volume or those seeking quick restoration. Their minimally invasive nature makes them particularly suitable for elderly, medically compromised, or surgery-averse individuals. However, patients must adhere strictly to post-operative care instructions and attend regular follow-ups to ensure long-term implant stability. In complex cases (such as severe bone loss), traditional implants or bone grafting procedures may still be necessary for optimal restoration outcomes.
Why Choose Mini Dental Implants?
1. Ideal for Patients with Low Bone Volume
With a diameter of only 2-3mm, mini dental implants can be placed in the superficial layer of the jawbone or in shallower areas without requiring additional bone grafting. This makes them a viable solution for patients with osteoporosis or those who have experienced bone resorption due to long-term tooth loss.
2. Minimally Invasive & Quick Recovery
Mini implants involve a less invasive procedure with no need for flap surgery or sutures. In some cases, the implant and prosthetic restoration can be completed on the same day. With minimal post-operative pain and a fast recovery period, they are particularly suitable for elderly or medically compromised patients.
3. Immediate Loading Capability
Thanks to their ball-and-socket design, mini implants can support immediate or light-load chewing in certain areas. This reduces the duration of edentulism, significantly improving the patient’s quality of life.
4. Cost-Effective Solution
The simplified surgical procedure and shorter treatment timeline reduce both material and labor costs. This makes mini dental implants a budget-friendly option for patients seeking a quick and affordable solution for both function and aesthetics.
5. Flexibility & Reversibility
If a future transition to traditional implants or a different restorative approach is needed, mini implants can be relatively easily removed, leaving room for alternative treatments.
Mini Dental Implant Care Guide
Caring for mini dental implants follows three key principles: daily cleaning, professional maintenance, and risk prevention. Despite their natural appearance and functionality, proper care is essential for the longevity of your implants. By maintaining daily hygiene, scheduling regular check-ups, and avoiding harmful habits, you can maximize the lifespan of your implants and restore your confident smile.
1. Daily Cleaning
Brushing:
Use a soft or extra-soft toothbrush to clean the implants and surrounding gums gently twice a day, in the morning and evening. Avoid vigorous brushing to prevent damage to the surgical site.
If the gums are sensitive post-surgery, fluoride toothpaste can help enhance cavity prevention.
Dental Floss & Interdental Brushes:
Use dental floss or a mini interdental brush daily to clean between the implants and adjacent teeth to prevent food buildup.
For removable prosthetics (if applicable), remove and gently wipe the implant abutment and surrounding soft tissues with a soft cotton swab dipped in toothpaste.
2. Professional Maintenance
Dental Check-ups:
Visit your dentist every 6 months for an implant stability assessment, plaque evaluation, and panoramic X-rays to detect any signs of loosening, bone resorption, or infection early.
Deep Cleaning:
Your dentist will use professional tools to remove hardened plaque (tartar) around the implant, helping to prevent peri-implantitis (implant infection).
3. Special Care: Post-Surgery Sensitivity Management
Initial Post-Surgery (1-2 weeks):
Avoid hot, cold, or spicy foods to reduce irritation to the gums.
If there is redness, swelling, or mild bleeding, use an antibacterial mouthwash recommended by your doctor (such as chlorhexidine) to help reduce inflammation.
Long-Term Maintenance:
Quit smoking, limit alcohol consumption, and manage systemic conditions like diabetes to reduce the risk of implant failure.
Avoid chewing hard objects (such as nuts or bottle caps) with the implants to prevent excessive loading, which may cause screw loosening or ceramic breakage.
Conclusion
With its “small size, big impact” breakthrough design, mini dental implants bring precision and minimally invasive innovation to the field of tooth restoration. Their core value lies not only in overcoming bone volume limitations with a 2-3mm compact structure but also in offering minimally invasive procedures (reducing surgical trauma by 30%), immediate loading capability, and short treatment cycles (some cases allowing same-day tooth placement). These features make them an ideal solution for patients with insufficient bone volume, advanced age, diabetes, or low surgical tolerance. Compared to traditional implants, mini implants redefine the boundaries of tooth restoration with lower invasiveness and higher adaptability, serving as a valuable complement rather than a replacement for conventional solutions.
The rise of mini dental implants marks a shift in tooth restoration from a “one-size-fits-all” approach to a personalized and precise paradigm. This is not just a technological advancement but also a progression in dental care philosophy—by minimizing trauma and maximizing patient comfort, more individuals can regain a fully functional and natural-looking smile. As material science and digital technology continue to evolve, mini dental implants are expected to expand their indications, solidifying their role as an essential precision dental tool. Both patients and dental professionals should embrace this innovation with an open mind, exploring the most suitable restoration pathways tailored to individual needs.